Primary Liver / Hepatic Cancer
Your Body is Your Temple
Research, Resources & Education
Table of Contents
Liver cancer is a disease that occurs when there is an abnormal growth of cancer cells in the liver tissue. This condition is also referred to as primary hepatic cancer or malignancy. It is essential to seek medical attention as soon as possible if you notice any symptoms of liver cancer, such as jaundice, abdominal pain, or unexplained weight loss. There are various treatment options available, depending on the stage and severity of the cancer, which can include surgery, radiation therapy, and chemotherapy.
Information and pictures from National Cancer Institute unless otherwise specified
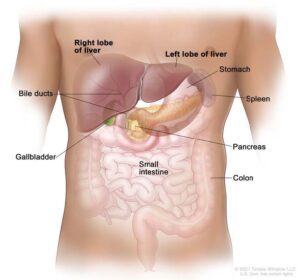
Types of Liver Cancer and Liver Anatomy
There are two types of adult primary liver cancer.
- Hepatocellular carcinoma – Most common
- Cholangiocarcinoma (bile duct cancer).
The liver is one of the largest organs in the body. It has two lobes and fills the upper right side of the abdomen inside the rib cage.
Three of the many important functions of the liver are:
- To filter harmful substances from the blood so they can be passed from the body in stools and urine.
- To make bile to help digest fat that comes from food.
- To store glycogen (sugar), which the body uses for energy.
Liver Cancer Videos
YouTube Videos that help explain types of Liver Cancer.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Liver Cancer
0:16
Treatments for Liver Cancer
Also see Treatments
- A partial hepatectomy (surgery to remove the part of the liver where cancer is found) may be done.
- A wedge of tissue, an entire lobe, or a larger part of the liver, along with some of the healthy tissue around it is removed.
- The remaining liver tissue takes over the functions of the liver and may re-grow.
- Total Hepatectomy with Liver transplant: In a liver transplant, the entire liver is removed and replaced with a healthy donated liver.
- A liver transplant may be done when the disease is in the liver only and a donated liver can be found.
- If the patient has to wait for a donated liver, other treatment is given as needed.
Possible side effect is rejection of the liver.
- Other side effects may be specific to drugs given.
- Immediately call your doctor if you experience a fever, redness or pus at your surgery site, bleeding or signs of liver failure – yellowing of the skin or whites of the eyes, dark urine or confusion – after surgery.
Ablation therapy removes or destroys tissue. Different types of ablation therapy are used for liver cancer:
- Radiofrequency ablation: The use of special needles that are inserted directly through the skin or through an incision in the abdomen to reach the tumor.
- High-energy radio waves heat the needles and tumor which kills cancer cells.
- Microwave therapy: A type of treatment in which the tumor is exposed to high temperatures created by microwaves.
- This can damage and kill cancer cells or make them more sensitive to the effects of radiation and certain anticancer drugs.
- Percutaneous ethanol injection: A cancer treatment in which a small needle is used to inject ethanol (pure alcohol) directly into a tumor to kill cancer cells.
- Several treatments may be needed.
- Usually local anesthesia is used, but if the patient has many tumors in the liver, general anesthesia may be used.
- Cryoablation: A treatment that uses an instrument to freeze and destroy cancer cells.
- This type of treatment is also called cryotherapy and cryosurgery.
- The doctor may use ultrasound to guide the instrument.
- Electroporation therapy: A treatment that sends electrical pulses through an electrode placed in a tumor to kill cancer cells.
- Electroporation therapy is being studied in clinical trials.
The use of substances to block or decrease the flow of blood through the hepatic artery to the tumor.
- When the tumor does not get the oxygen and nutrients it needs, it will not continue to grow.
- Embolization therapy is used for patients who cannot have surgery to remove the tumor or ablation therapy and whose tumor has not spread outside the liver.
- The liver receives blood from the hepatic portal vein and the hepatic artery.
- Blood that comes into the liver from the hepatic portal vein usually goes to the healthy liver tissue.
- Blood that comes from the hepatic artery usually goes to the tumor.
- When the hepatic artery is blocked during embolization therapy, the healthy liver tissue continues to receive blood from the hepatic portal vein.
There are two main types of embolization therapy: - Transarterial embolization (TAE): A small incision (cut) is made in the inner thigh and a catheter (thin, flexible tube) is inserted and threaded up into the hepatic artery.
- Once the catheter is in place, a substance that blocks the hepatic artery and stops blood flow to the tumor is injected.
- Transarterial chemoembolization (TACE): This procedure is like TAE except an anticancer drug is also given.
- The procedure can be done by attaching the anticancer drug to small beads that are injected into the hepatic artery or by injecting the anticancer drug through the catheter into the hepatic artery and then injecting the substance to block the hepatic artery.
- Most of the anticancer drug is trapped near the tumor and only a small amount of the drug reaches other parts of the body.
- This type of treatment is also called chemoembolization.
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells.
- Targeted therapies usually cause less harm to normal cells than chemotherapy or radiation therapy do.
- Tyrosine kinase inhibitors are a type of targeted therapy used in the treatment of adult primary liver cancer.
- Tyrosine kinase inhibitors are small-molecule drugs that go through the cell membrane and work inside cancer cells to block signals that cancer cells need to grow and divide.
- Some tyrosine kinase inhibitors also have angiogenesis inhibitor effects.
- Sorafenib, lenvatinib, regorafenib, and cabozantinib are types of tyrosine kinase inhibitors used to treat advanced liver cancer.
Immunotherapy is a treatment that uses the patient’s immune system to fight cancer.
- Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defenses against cancer.
- This cancer treatment is a type of biologic therapy.
- Immune checkpoint inhibitor therapy is a type of immunotherapy.
- PD-1 and PD-L1 inhibitor therapy: PD-1 is a protein on the surface of T cells that helps keep the body’s immune responses in check.
- PD-L1 is a protein found on some types of cancer cells.
- When PD-1 attaches to PD-L1, it stops the T cell from killing the cancer cell. PD-1 and PD-L1 inhibitors keep PD-1 and PD-L1 proteins from attaching to each other.
- This allows the T cells to kill cancer cells.
- Pembrolizumab is a type of PD-1 inhibitor.
Radiation therapy
Targeted therapy
Treatment by Type of Cancer
Also see Treatments
Treatment of localized adult primary liver cancer may include the following:
- Surveillance for lesions smaller than 1 centimeter.
- Partial hepatectomy.
- Total hepatectomy and liver transplant.
- Ablation of the tumor using one of the following methods:
- Radiofrequency ablation.
- Microwave therapy.
- Percutaneous ethanol injection.
- Cryoablation.
- A clinical trial of electroporation therapy.
Treatment of locally advanced or metastatic adult primary liver cancer that cannot be treated with surgery may include the following:
- Embolization therapy using transarterial embolization (TAE) or transarterial chemoembolization (TACE).
- Targeted therapy with sorafenib, lenvatinib, regorafenib, or cabozantinib.
- Immune checkpoint inhibitor therapy with pembrolizumab.
- Radiation therapy.
- A clinical trial of targeted therapy after chemoembolization or combined with chemotherapy.
- A clinical trial of new targeted therapy drugs.
- A clinical trial of immunotherapy.
- A clinical trial of immunotherapy combined with targeted therapy.
- A clinical trial of stereotactic body radiation therapy or proton-beam radiation therapy.
Treatment options for recurrent adult primary liver cancer may include the following:
- Total hepatectomy and liver transplant.
- Partial hepatectomy.
- Ablation.
- Transarterial chemoembolization and targeted therapy with sorafenib, as palliative therapy to relieve symptoms and improve quality of life.
Risk Factors / Possible Side Effects or Complications
Risk Factors
- Having hepatitis B or hepatitis C.
- Having cirrhosis, which can be caused by: hepatitis (especially hepatitis C)
- Drinking large amounts of alcohol for many years or being an alcoholic.
- Having metabolic syndrome,
- Having liver injury that is long-lasting
- Having hemochromatosis
- Eating foods tainted with aflatoxin (poison from a fungus that can grow on foods)
Side Effects / Complications
Liver transplant surgery carries a risk of significant complications. There are risks associated with the procedure itself as well as with the drugs necessary to prevent rejection of the donor liver after the transplant.
Risks associated with the procedure include:
- Bile duct complications, including bile duct leaks or shrinking of the bile ducts
- Bleeding
- Blood clots
- Failure of donated liver Infection
- Rejection of donated liver
- Mental confusion or seizures
- Long-term complications may also include recurrence of liver disease in the transplanted liver.
Anti-rejection medication side effects
After a liver transplant, you’ll take medications for the rest of your life to help prevent your body from rejecting the donated liver.
These anti-rejection medications can cause a variety of side effects, including:
- Bone thinning
- Diabetes
- Diarrhea
- Headaches
- High blood pressure
- High cholesterol
- Because anti-rejection drugs work by suppressing the immune system, they also increase your risk of infection. Your doctor may give you medications to help you fight infections.
Recovery after Surgery
Information from CETI
Please follow MD/surgeon protocol, as every situation is unique.
Partial Hepatectomy
Hospital Stay
Full Recovery
Restrictions
Exercise
Total Hepatectomy with Liver Transplant
Hospital Stay
Full Recovery
Restrictions
Exercise
Exercise and Sports Participation
4.3 Sports participation – Physiotherapy in Liver Transplantation
Long Term After 3 Months
- Sports participation after solid organ transplantation is the final objection of the long-term rehabilitation process for maximizing quality of life. It is recommended to encourage the patients to participate in a sports activity three months after the surgery. This time is required to achieve optimal flexibility, muscular strength, muscular endurance and aerobic capacity and to provide proper post-operative wound healing and graft stabilization so that the patient can do sports without any deterioration.
- Patients should start with light activities such as walking, stair climbing, golf, bowling, darts, archery and fishing. Table tennis and volleyball can be suggested as medium intensity activities. Swimming, athletics, badminton, cycling, rowing, squashes, tennis, mini-marathon are recommended after getting used to light and moderate activities.
- However, swimming in community pools or lakes is not recommended because of high risk of infectious organisms. High impact and contact sports such as football, basketball, horse riding and bungee jumping are not preferable as they may cause a serious trauma and lead to organ damage. Patients usually have a fear of organ damage or severe pain avoiding them to participate in sports.
- Contact sports also have an additional fracture risk for weight bearing bones due to long term osteoporotic effects of corticosteroids. As liver transplantation surgery induces a denervation of the liver and intrahepatic vascular system strenuous exercises may carry a high risk for reduction in portal blood flow due to increased demands of contracting muscles (Ersoz&Ersoz, 2003).
- Besides, selected and well-prepared liver transplant recipients were able to participate in mountain trek and tolerate exposure to high altitude similar to healthy subjects after a 6-month aerobic training and a hypercaloric diet including sugars, proteins and abundant hydration (Pirenne et al., 2004).
- Feeling of distress, muscle and joint pain, incisional pain and fatigue are the complaints of transplant recipients during or after exercises. Running, skiing, bike riding and tennis, shotput and bodybuilding were reported as the most popular sports among a group of patients with liver and kidney transplantation (Pupkal et al., 2008).
- Patients may participate in a sport not only for a leisure time activity but also for professional competitions. The World Transplant Games Federation, officially recognized by the International Olympic Committee, is a world-wide organization staging international sporting events for transplant athletes for over 20 years in order to demonstrate the ability of sports participation after organ transplantation and to raise awareness of the vitality of organ donation.
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
Information and pictures from National Cancer Institute unless otherwise specified