Breast Cancer Surgeries & Reconstruction
Your Body is Your Temple
Research, Resources & Education
Table of Contents
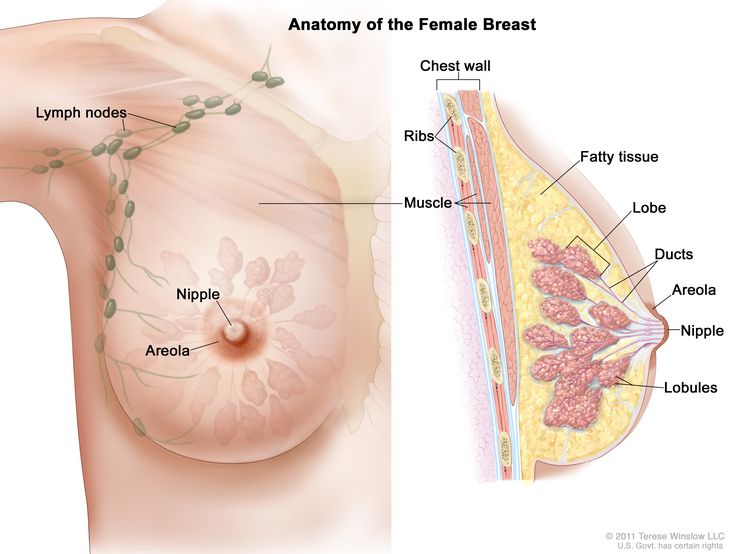
Breast cancer requires careful consideration of surgeries including mastectomy, lumpectomy, and nipple sparing. Each surgery has benefits and risks that affect patient outcomes. Post-surgery reconstruction may also be necessary and requires a consultation with a qualified healthcare professional. Well-being in physical, emotional, and psychological realms must be a priority in all cases.
Information and pictures from National Cancer Institute unless otherwise specified
Types of Breast Surgeries & Reconstruction Videos
YouTube Videos that help explain different types of Breast Surgeries & Reconstruction Options.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Breast Surgery & Reconstruction
Mastectomy
Information from the Dept. Of Health, NY: Breast Cancer Treatment
Surgical removal of the breast that has DCIS or cancer. There are different types of mastectomies:
- Total mastectomy (also known as simple mastectomy)
- Skin-sparing mastectomy
- Modified radical mastectomy.
A mastectomy is most often recommended when:
- There are multiple areas of cancer within your breast
- The tumor is greater than 5cm (2inches)
- Your breast is small or shaped such that removal of the entire cancer will leave little breast tissue or a deformed breast
- You do not want or cannot have radiation therapy (sometimes radiation is necessary, even if you have a mastectomy).
Possible Side Effects of Mastectomy
- Infection, poor wound healing, a reaction to the drugs used in surgery (anesthesia)
- A collection of fluid or blood under the skin may occur after a mastectomy
(Department of Health NY: Breast Cancer Treatment)
Breast Conserving Lumpectomy
Also called breast-sparing surgery, partial mastectomy, quadrantectomy or segmental mastectomy.
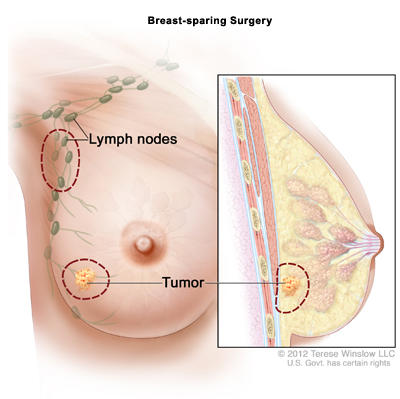
Breast-sparing surgery means the surgeon removes only the DCIS or cancer and some normal tissue around it.
- If you have cancer, the surgeon will also remove one or more lymph nodes from under your arm.
- Breast-sparing surgery usually keeps your breast looking much like it did before surgery.
- After breast-sparing surgery, most women also receive radiation therapy. Some women will also need chemotherapy, hormone therapy, and/or targeted therapy.
- The main goal of this treatment is to keep cancer from coming back in the same breast.
Is this surgery right for me?
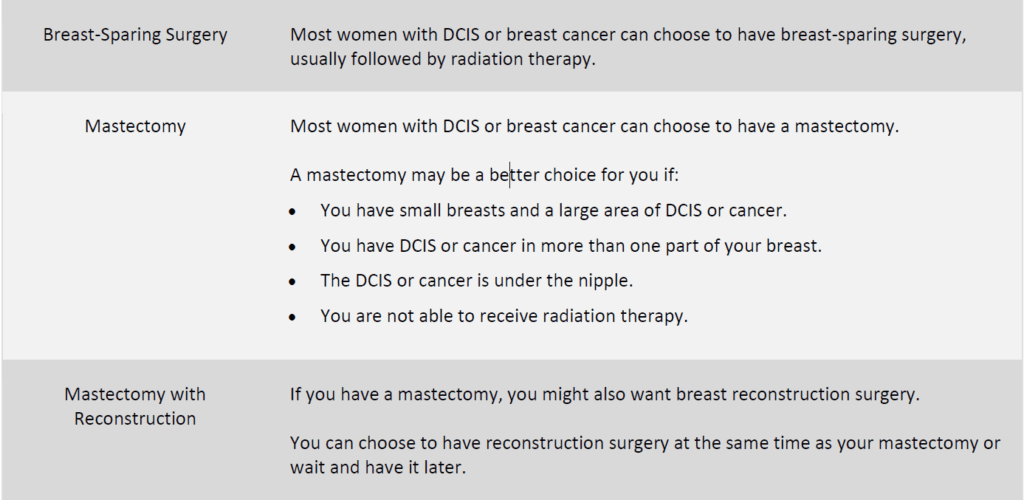
- Most women with DCIS or breast cancer can choose to have breast-sparing surgery, usually followed by radiation therapy.
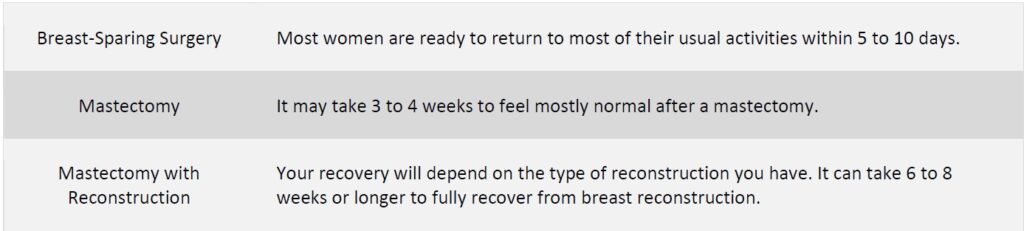
How long before I can return to normal activities?
- Most women are ready to return to most of their usual activities within 5 to 10 days.
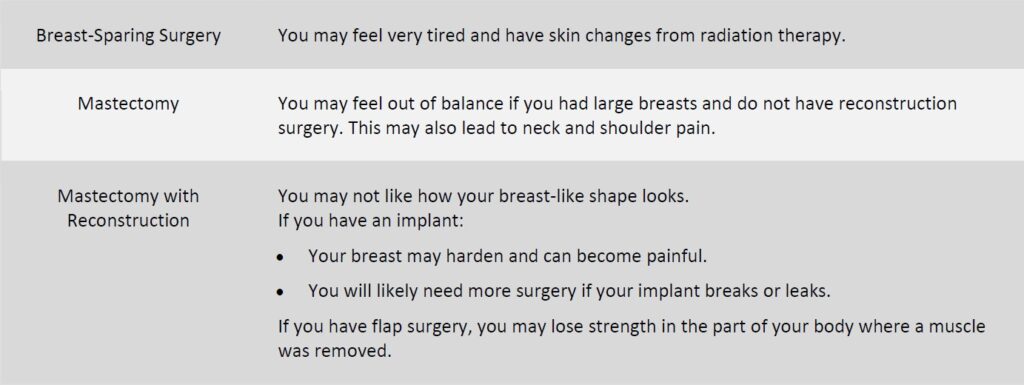
What other problems might I have?
- You may feel very tired and have skin changes from radiation therapy.
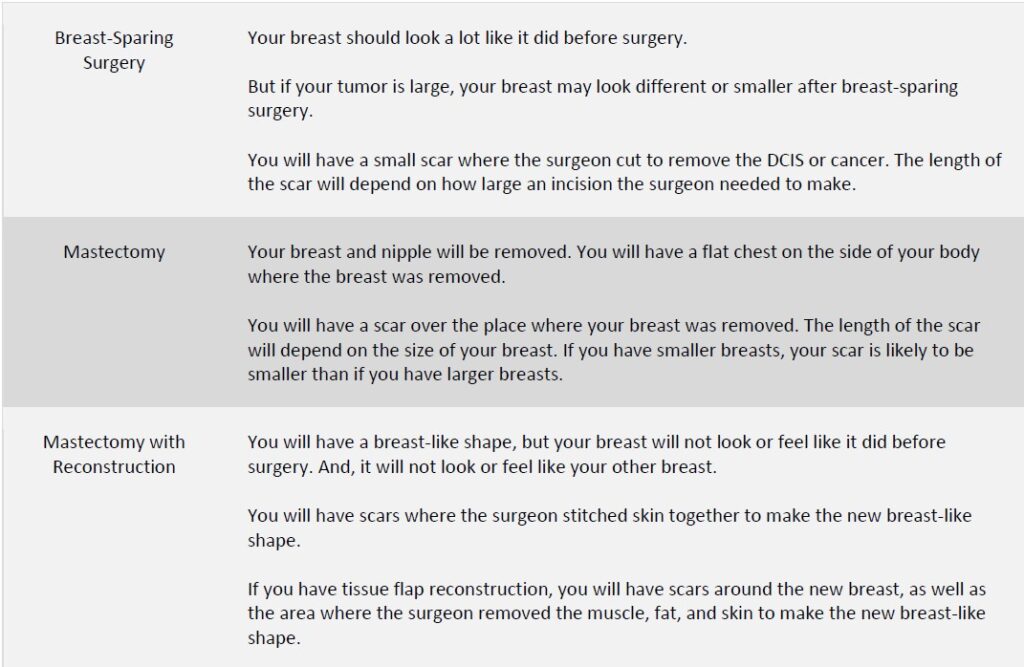
What will my breast look like?
- Your breast should look a lot like it did before surgery.
- But if your tumor is large, your breast may look different or smaller after breast-sparing surgery.
- You will have a small scar where the surgeon cut to remove the DCIS or cancer.
- The length of the scar will depend on how large an incision the surgeon needed to make.
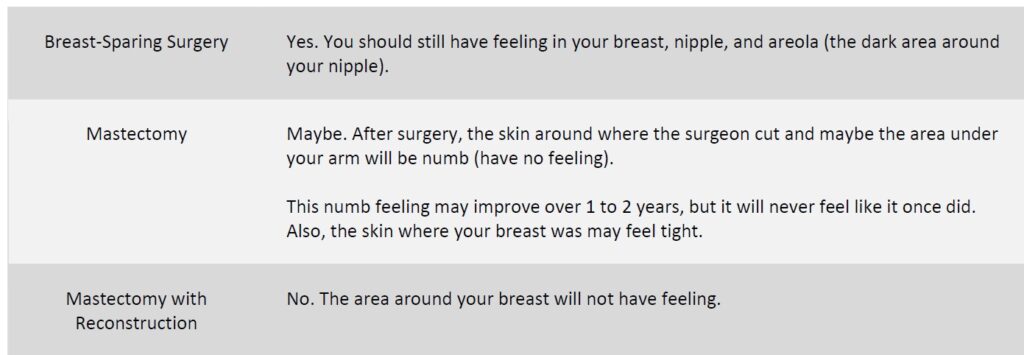
Will my breast have feeling?
- Yes. You should still have feeling in your breast, nipple, and areola (the dark area around your nipple).
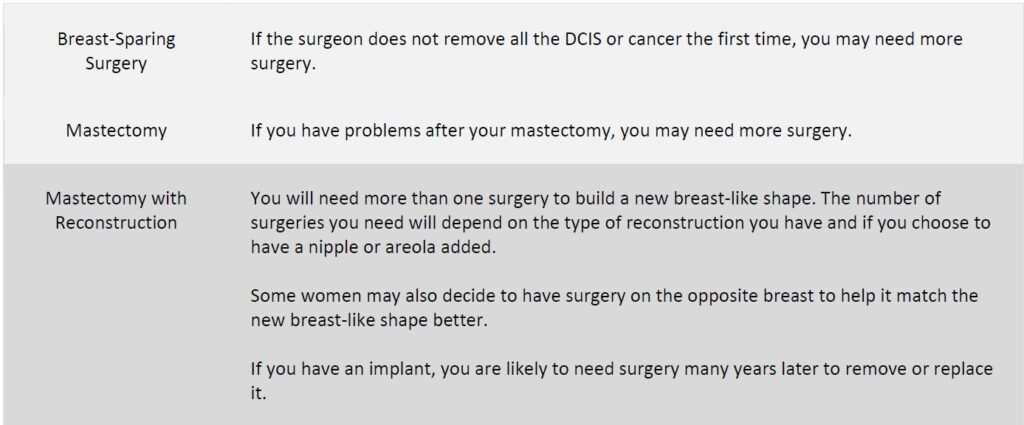
Will I need more surgery?
- If the surgeon does not remove all the DCIS or cancer the first time, you may need more surgery.
What are the chances that my breast cancer will return in the same area?
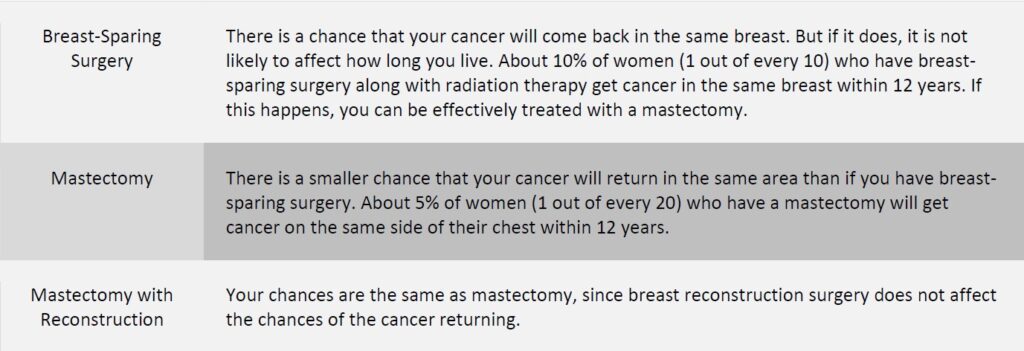
- There is a chance that your cancer will come back in the same breast. But if it does, it is not likely to affect how long you live.
- About 10% of women (1 out of every 10) who have breast-sparing surgery along with radiation therapy get cancer in the same breast within 12 years.
- If this happens, you can be effectively treated with a mastectomy.(NCI)
Nipple Sparing Mastectomy
A nipple-sparing mastectomy is similar to the skin-sparing mastectomy.
- This procedure is more often an option for women who have a small, early-stage cancer near the outer part of the breast, with no signs of cancer in the skin or near the nipple.
- The surgeon often removes the breast tissue beneath the nipple (and areola) during the procedure, to check for cancer cells.
- If cancer is found in this tissue, the nipple must be removed.
(Department of Health NY: Breast Cancer Treatment)
Total Mastectomy or Simple Mastectomy
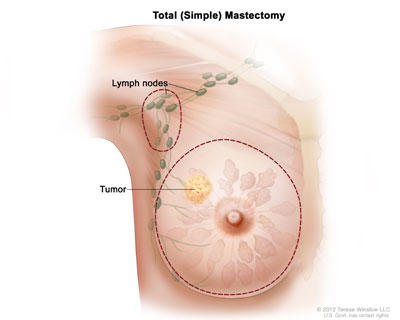
The surgeon removes your whole breast.
- Sometimes, the surgeon also takes out one or more of the lymph nodes under your arm.
Modified Radical Mastectomy
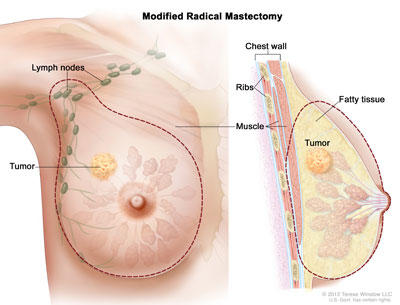
Surgery for breast cancer in which the breast, most or all of the lymph nodes under the arm, and the lining over the chest muscles are removed.
- Sometimes the surgeon also removes part of the chest wall muscles.
Considerations with Mastectomy & Reconstruction
Is this surgery right for me?
- Most women with DCIS or breast cancer can choose to have a mastectomy.
- A mastectomy may be a better choice for you if:
- You have small breasts and a large area of DCIS or cancer.
- You have DCIS or cancer in more than one part of your breast.
- The DCIS or cancer is under the nipple.
- You are not able to receive radiation therapy.
How long before I can return to normal activities?
- It may take 3 to 4 weeks to feel mostly normal after a mastectomy.
What other problems might I have?
- You may feel out of balance if you had large breasts and do not have reconstruction surgery.
- This may also lead to neck and shoulder pain.
What will my breast look like?
- Your breast and nipple will be removed.
- You will have a flat chest on the side of your body where the breast was removed.
- You will have a scar over the place where your breast was removed.
- The length of the scar will depend on the size of your breast.
- If you have smaller breasts, your scar is likely to be smaller than if you have larger breasts.
Will my breast have feeling
- Maybe. After surgery, the skin around where the surgeon cut and maybe the area under your arm will be numb (have no feeling).
- This numb feeling may improve over 1 to 2 years, but it will never feel like it once did.
- Also, the skin where your breast was may feel tight.
Will I need more surgery?
- If you have problems after your mastectomy, you may need more surgery.
What are the chances that my breast cancer will return in the same area?
- There is a smaller chance that your cancer will return in the same area than if you have breast-sparing surgery.
- About 5% of women (1 out of every 20) who have a mastectomy will get cancer on the same side of their chest within 12 years. (NCI)
Is this surgery right for me?
- If you have a mastectomy, you might also want breast reconstruction surgery.
You can choose to have reconstruction surgery at the same time as your mastectomy or wait and have it later.
How long before I can return to normal activities?
- Your recovery will depend on the type of reconstruction you have.
- It can take 6 to 8 weeks or longer to fully recover from breast reconstruction.
What other problems might I have?
- You may not like how your breast-like shape looks.
- If you have an implant:
- Your breast may harden and can become painful.
- You will likely need more surgery if your implant breaks or leaks.
- If you have flap surgery, you may lose strength in the part of your body where a muscle was removed.
What will my breast look like?
- You will have a breast-like shape, but your breast will not look or feel like it did before surgery.
- And, it will not look or feel like your other breast.
- You will have scars where the surgeon stitched skin together to make the new breast-like shape.
- If you have tissue flap reconstruction, you will have scars around the new breast, as well as the area where the surgeon removed the muscle, fat, and skin to make the new breast-like shape.
Will my breast have feeling?
- No. The area around your breast will not have feeling.
Will I need more surgery?
- You will need more than one surgery to build a new breast-like shape.
- The number of surgeries you need will depend on the type of reconstruction you have and if you choose to have a nipple or areola added.
- Some women may also decide to have surgery on the opposite breast to help it match the new breast-like shape better.
- If you have an implant, you are likely to need surgery many years later to remove or replace it.
What are the chances that my breast cancer will return in the same area?
- Your chances are the same as mastectomy, since breast reconstruction surgery does not affect the chances of the cancer returning.
(NCI)
Considering Different Types of Breast Surgery
Information from National Cancer Institute
|
Is this surgery right for me?
How long before I can return to normal activities?
What other problems might I have?
What will my breast look like?
Will my breast have feeling?
Will I need more surgery?
What are the chances that my breast cancer will return in the same area?
Breast Reconstruction, Timing & Methods
Many women who have a mastectomy surgery to remove an entire breast to treat or prevent breast cancer have the option of having the shape of the removed breast rebuilt.
- Women who choose to have their breasts rebuilt have several options for how it can be done.
- Breasts can be rebuilt using implants (saline or silicone).
- They can also be rebuilt using autologous tissue (that is, tissue from elsewhere in the body).
- Sometimes both implants and autologous tissue are used to rebuild the breast.
- Surgery to reconstruct the breasts can be done (or started) at the time of the mastectomy (which is called immediate reconstruction) or it can be done after the mastectomy incisions have healed and breast cancer therapy has been completed (which is called delayed reconstruction).
- Delayed reconstruction can happen months or even years after the mastectomy. •
- In a final stage of breast reconstruction, a nipple and areola may be re-created on the reconstructed breast, if these were not preserved during the mastectomy.
- Sometimes breast reconstruction surgery includes surgery on the other, or contralateral, breast so that the two breasts will match in size and shape.
- One factor that can affect the timing of breast reconstruction is whether a woman will need radiation therapy.
- Radiation therapy can sometimes cause wound healing problems or infections in reconstructed breasts, so some women may prefer to delay reconstruction until after radiation therapy is completed.
- However, because of improvements in surgical and radiation techniques, immediate reconstruction with an implant is usually still an option for women who will need radiation therapy.
- Autologous tissue breast reconstruction is usually reserved for after radiation therapy, so that the breast and chest wall tissue damaged by radiation can be replaced with healthy tissue from elsewhere in the body.
- Another factor is the type of breast cancer.
- Women with inflammatory breast cancer usually require more extensive skin removal
- This can make immediate reconstruction more challenging, so it may be recommended that reconstruction be delayed until after completion of adjuvant therapy.
- Even if a woman is a candidate for immediate reconstruction, she may choose delayed reconstruction.
- For instance, some women prefer not to consider what type of reconstruction to have until after they have recovered from their mastectomy and subsequent adjuvant treatment.
- Women who delay reconstruction (or choose not to undergo the procedure at all) can use external breast prostheses, or breast forms, to give the appearance of breasts.
Surgery and recovery
- Enough skin and muscle must remain after mastectomy to cover the implants
- Shorter surgical procedure than for reconstruction with autologous tissue; little blood loss
- Recovery period may be shorter than with autologous reconstruction
- Many follow-up visits may be needed to inflate the expander and insert the implant
Possible complications
- Infection
- Accumulation of clear fluid causing a mass or lump (seroma) within the reconstructed breast
- Pooling of blood (hematoma) within the reconstructed breast
- Blood clots
- Extrusion of the implant (the implant breaks through the skin)
- Implant rupture (the implant breaks open and saline or silicone leaks into the surrounding tissue)
- Formation of hard scar tissue around the implant (known as a contracture) diabetes, and smoking may increase the rate of complications
- Possible increased risk of developing a very rare form of immune system cancer called anaplastic large cell lymphoma
Other considerations
- May not be an option for patients who have previously undergone radiation therapy to the chest
- May not be adequate for women with very large breasts
- Will not last a lifetime; the longer a woman has implants, the more likely she is to have complications and to need to have her implants removed or replaced
- Silicone implants may feel more natural than saline implants to the touch
- The Food and Drug Administration (FDA) recommends that women with silicone implants undergo periodic MRI screenings to detect possible “silent” rupture of the implants.
Reconstruction with Implants vs. Autologous Tissue
Surgery and recovery
- Longer surgical procedure than for implants
- The initial recovery period may be longer than for implants
- Pedicled flap reconstruction is usually a shorter operation than free flap reconstruction and usually requires a shorter hospitalization
- Free flap reconstruction is a longer, highly technical operation compared with pedicled flap reconstruction that requires a surgeon who has experience with microsurgery to re-attach blood vessels
Possible complications
- Necrosis (death) of the transferred tissue
- Blood clots may be more frequent with some flap sources
- Pain and weakness at the site from which the donor tissue was taken
- Obesity, diabetes, and smoking may increase the rate of complications
Other considerations
- May provide a more natural breast shape than implants
- May feel softer and more natural to the touch than implants
- Leaves a scar at the site from which the donor tissue was taken
- Can be used to replace tissue that has been damaged by radiation therapy.
Surgery and recovery
- Longer surgical procedure than for implants
- The initial recovery period may be longer than for implants
- Pedicled flap reconstruction is usually a shorter operation than free flap reconstruction and usually requires a shorter hospitalization
- Free flap reconstruction is a longer, highly technical operation compared with pedicled flap reconstruction that requires a surgeon who has experience with microsurgery to re-attach blood vessels
Possible complications
- Necrosis (death) of the transferred tissue
- Blood clots may be more frequent with some flap sources
- Pain and weakness at the site from which the donor tissue was taken
- Obesity, diabetes, and smoking may increase the rate of complications
Other considerations
- May provide a more natural breast shape than implants
- May feel softer and more natural to the touch than implants
- Leaves a scar at the site from which the donor tissue was taken
- Can be used to replace tissue that has been damaged by radiation therapy.
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
Information and pictures from National Cancer Institute unless otherwise specified