Cancer: Starting an Exercise Program, Guidelines & Risks
Your Body is Your Temple
Research, Resources & Education
Table of Contents
It is crucial to gather information regarding your activity levels before cancer treatment and to assess any potential risks associated with initiating a physical exercise routine. It is recommended to consult with your healthcare provider or a trained professional in order to determine the most appropriate approach for your individual situation. This may involve taking into account factors such as the type and stage of cancer, any past surgeries or treatments received, and any physical limitations or side effects experienced.
Information and pictures from National Cancer Institute unless otherwise specified
Although this website is about Cancer & Exercise Programs, it is extremely important to follow your oncology team’s prescription, especially after surgery. All cancer treatments are different and each doctor will have their particular protocol to follow. It may be necessary to participate in physical therapy first and use this book as a guide along with their program. It is also very important to be cleared from a specialist for other complications, such as, but not limited to, heart disease, pulmonary disease, diabetes, bone disease, immune disorders, obesity or neurological conditions.
Starting an Exercise Program
Cancer Survivors:
If you have finished your treatments, have no comorbiditIes or any precautions or contraindications to exercise, You should still continue to follow recommendations from your oncology team or physical therapist, and the follow along with the exercise programs for a healthy adult. You may need to progress at a slower rate, especially if you were physically active prior to your treatments, but be patient and don’t give up.
Exercise Guidelines for Cancer patients currently receiving treatment:
The following information includes research from:
National Comprehensive Cancer Network (NCCN) – Exercising During Cancer Treatments
American Cancer Society – Physical Activity and the Cancer Patient
- American Cancer Society: “To make your exercise effort most effective (give you the best results), it’s important that you work your heart. Notice your heart rate, your breathing, and how tired your muscles get.
- If you get short of breath or very tired, rest for a few seconds, and start exercising again as you are able.
- When you first start, the goal is to exercise for at least 10 minutes at a time.
- Go slow at first, and over the next few weeks, increase the length of time you exercise.
- Be careful if you’re taking blood pressure medicine that controls your heart rate. Your heart rate will not go up, but your blood pressure can get high. Ask your doctor, nurse, or pharmacist about this if you’re not sure about your medicines.
- We don’t know the best level of exercise for someone with cancer. The goal is to have your exercise program help you keep up your muscle strength and keep you able to do the things you want and need to do.
- The more you exercise, the better you’ll be able to exercise and function.
- But even if planned exercise stops, it’s good to keep being active by doing your normal activities as much as you can”.
- Goal: At least 30 minutes of aerobic exercise five days a week or more.
- Start slowly and work your way up. For example, if you are taking a walk, try short periods and rest frequently. Start at a slow 5-10 minute walk, rest, and try a brisk 5 minutes.
- You can also split up your sessions into 10 minutes throughout the day to equal 30. You don’t have to start out at 30 minutes, but work up to it.
- Keep track of when you energy levels are at their highest.
- Pain and fatigue can change daily, but take advantage of the times when you are feeling the best.
- Try to keep on a daily routine.
- When you are feeling moderately fatigued, try getting up and doing something around the house to help with your endurance. It can be something as simple as walking up and down the hallway.
- Try getting up and walking hourly for circulation when you are not sleeping/napping.
- Balance activity with rest that does not interfere with nighttime sleep.
- Be flexible and listen to your body. Although you should keep some type of a schedule, don’t feel like you need to follow it strictly. If you are feeling ill, extremely fatigues or running a fever let your body rest.
- If you don’t feel like doing a regimented routine, try gardening, housework or any other physical hobby you may enjoy. Ask someone to walk with you or use headphones while exercising or walking.
- Drink about 8 to 10 glasses of water a day unless your doctor tells you not to.
- Unless you are told otherwise, eat a balanced diet that includes protein (meat, milk, eggs, and legumes such as peas or beans).
- Dress comfortably, especially in either cold or humid weather.
Exercise Guidelines
Information from the American Cancer Society – Physical Activity and the Cancer Patient and
Cancer Research UK – Exercise Guidelines for Cancer Patients unless otherwise specified
- May help to decrease nausea during chemotherapy
- May relieve constipation by stimulating digestion and elimination systems
- Increases endurance due to fatigue
- Help to keep or improve your physical abilities (how well you can use your body to do things)
- Improve balance, which may lower risk of falls and broken bones
- Keep muscles from wasting due to inactivity
- Decrease the risk of heart disease
- Decrease the risk of osteoporosis – helps to strength bones
- Improving blood flow to the legs, reducing the risk of blood clots
- Make you less dependent on others for help with normal activities of daily living
- Lower the risk of being anxious and depressed
- Help you control your weight
This makes a big difference in deciding how you will proceed with your exercise program.
- If you lead a sedentary lifestyle before the cancer, this is not the time to start a moderate aerobic exercise program.
- This does not mean you should not start an exercise program at all; you will just need to start at a basic level.
- On the other hand, if you were an athlete before your diagnosis, this will mean you need to cut back during treatment and eventually move forward to regain your strength.
- Pain, fatigue and possibly nausea are the most limiting factors during your treatment.
- Other factors could be peripheral neuropathy, which may alter your balance, dehydration or lymphedema, etc.
- Some people also have pre-existing or cancer caused comorbiditIes, (the presence of one or more additional diseases or disorders co-occurring with a primary disease or disorder), which could include heart disease, pulmonary disease, obesity, diabetes, neurological conditions or bone disease, among others.
- In this instance, you will have to speak to the team of doctors to discuss which exercises will be best suited for not only the cancer, but other comorbidity.
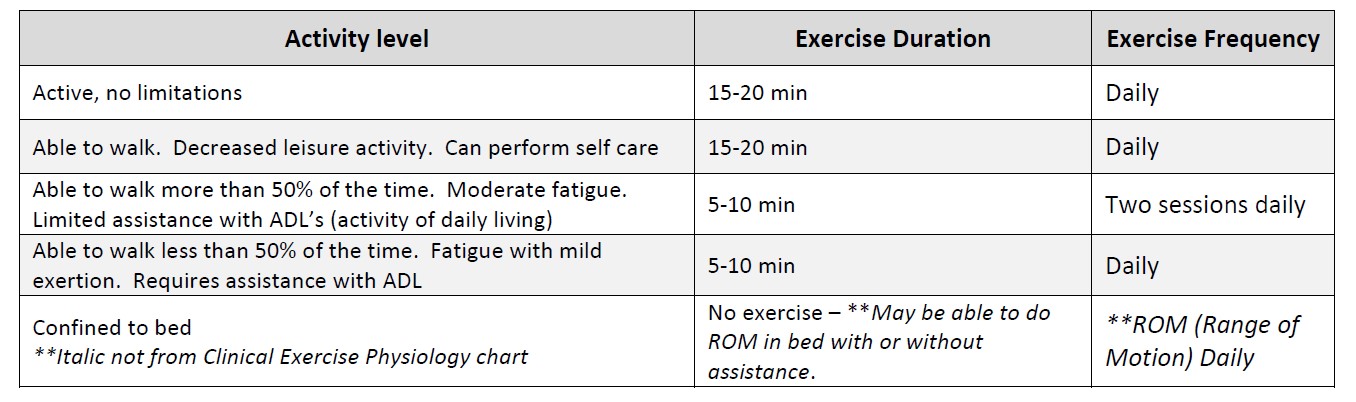
(Chart adapted from Clinical Exercise Physiology, pg. 440)
- Low red blood cell count (anemia).
- Low white blood cell counts or if you take medicines that make you less able to fight infection and impair your immune system.
- Stay away from public gyms and other public places until your counts are at a safe level.
- Abnormal level of minerals in your blood, such as sodium and potassium.
- This can happen if you have had a lot of vomiting or diarrhea.
- Unrelieved pain, nausea/vomiting, or any other symptom that causes you concern. Call your doctor.
- Do not exercise above a moderate level of exertion without talking with your doctor first.
- Remember, moderate exertion is about as much effort as a brisk walk.
- If you have a catheter or feeding tube, do not do resistance training that uses muscles in the area of the catheter to keep from dislodging it. Talk with your cancer team about what’s safe for you.
- Avoid pools, lakes, or ocean water and other exposures that may cause infections
- Skin irritation – people getting radiation should not expose skin in the treatment area to the chlorine in swimming pools.
- Avoid direct sunlight, even after radiation treatments are over due to burning.
- For radiation to the upper part of the body, suggest wearing a rash guard (shirt that has UV sun protection).
- Stay away from uneven surfaces or any weight-bearing exercises that could cause you to fall and hurt yourself.
- If you have cancer affecting your bones, you might be more at risk of a break or fracture.
- You must avoid putting too much strain on the affected bones.
- You could try swimming or exercising in water, as the water supports your body weight so the skeleton isn’t stressed.
- Do not use heavy weights or do exercise that puts too much stress on your bones if you have osteoporosis, cancer that has spread to the bone, arthritis, nerve damage, poor vision, poor balance, or weakness. You may be more likely to hurt yourself or break a bone.
- Watch for swollen ankles, unexplained weight gain, or shortness of breath while at rest or with a small amount of activity. Let your doctor know if you have any of these problems.
- Watch for lymphedema
- Watch for bleeding, especially if you are taking blood thinners.
- Avoid any activity that puts you at risk for falls or injury. If you notice swelling, pain, dizziness, or blurred vision, call your doctor right away.
- Peripheral neuropathy – Loss of sensation or feelings of pins and needles in your hands and feet due to cancer treatments.
- Because this puts you at a higher risk of falls, it might be better to use a stationary bike than to do other types of weight bearing exercise.
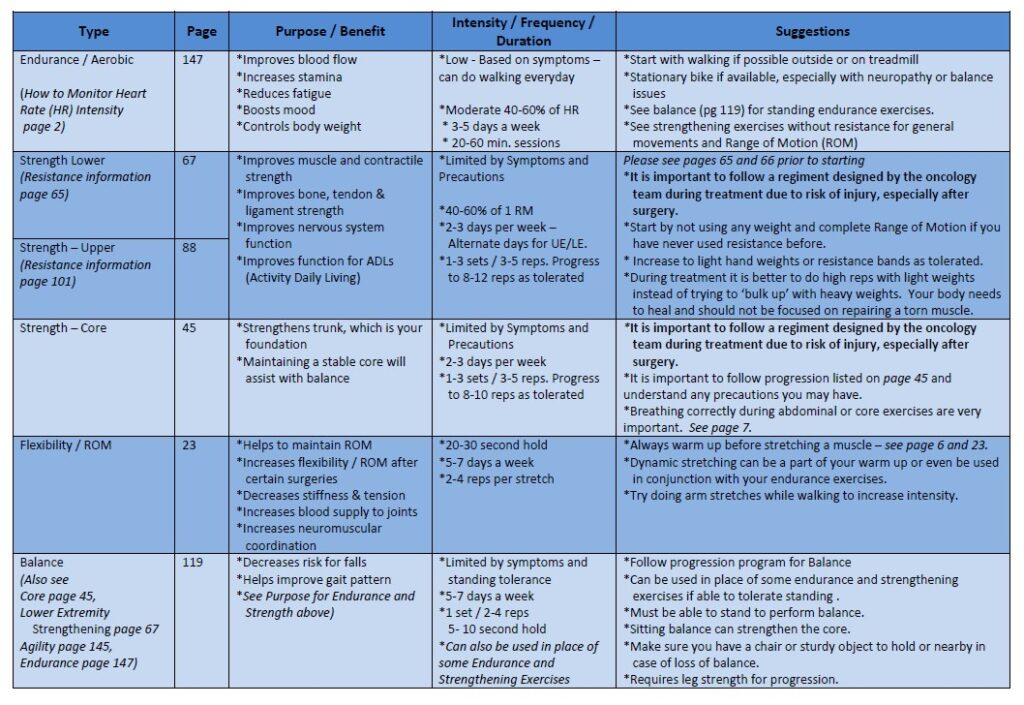
Guideline for Type of Exercise
Remember to always warm up before exercising and cool down if needed. This is especially true with flexibility training.
CETI Contraindications or Recommendations for Exercise
Information from CETI
Please follow MD/surgeon protocol, as every situation is unique.
PICC line
- Avoid resistance exercises around the PICC site
- Do not swim or play contact sports
- Avoid repetitive movements in the affected arm
Chemotherapy or Immunotherapy
- IV Chemotherapy – No exercise for 24 hours
- Hematocrit less than 25% – No Exercise
- Hemoglobin less than 24% 8g/dl due to anemia – No Exercise
- White blood cell counts less than 300 mm3 – No Exercise
- White blood cell counts – Avoid public gyms unless blood cell count is above 500 mm3
- Platelet count less than 5000 mm3 – No resistance training – risk of internal bleeding/hemorrhage
- Platelet count less than 30,000 mm3 – Gentle Active Range of Motion
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
Information and pictures from National Cancer Institute unless otherwise specified