Colon / Colorectal Cancer
Your Body is Your Temple
Research, Resources & Education
Table of Contents
Colorectal cancer is caused by polyps in the colon or rectum that become cancerous over time. Symptoms may not appear until late stages, so routine screening is crucial for early detection and treatment. Doctors may remove polyps during screenings to reduce the risk of cancer.
Information and pictures from National Cancer Institute unless otherwise specified
Colon Anatomy & Colon Cancer
Information on Colon Cancer from the CDC
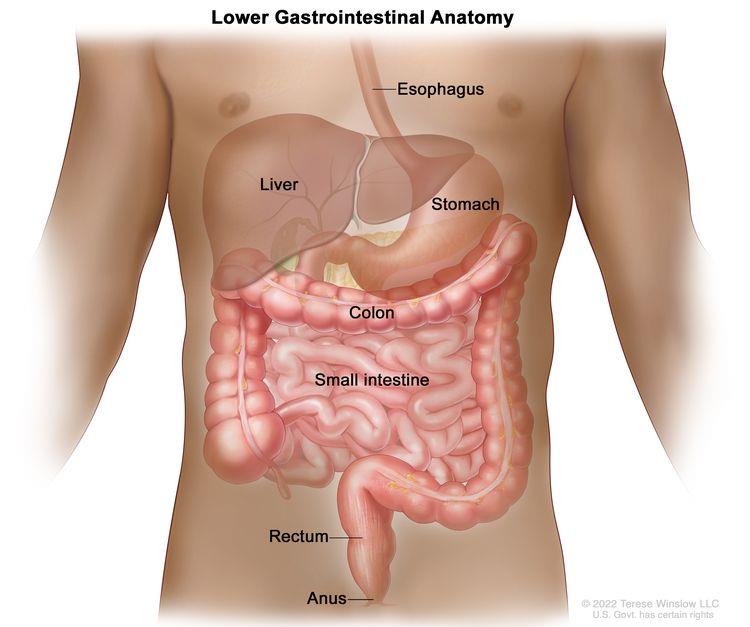
The colon is part of the body’s digestive system.
- The digestive system removes and processes nutrients (vitamins, minerals, carbohydrates, fats, proteins, and water) from foods and helps pass waste material out of the body.
- The digestive system is made up of the esophagus, stomach, and the small and large intestines.
- The colon (large bowel) is the first part of the large intestine and is about 5 feet long.
- Together, the rectum and anal canal make up the last part of the large intestine and are about 6-8 inches long.
- The anal canal ends at the anus (the opening of the large intestine to the outside of the body).
Cancer that forms in the tissues of the colon (the longest part of the large intestine).
- Most colon cancers are adenocarcinomas (cancers that begin in cells that make and release mucus and other fluids).
- Colorectal cancer is a disease in which cells in the colon or rectum grow out of control.
- Sometimes it is called colon cancer, for short.
- The colon is the large intestine or large bowel.
- The rectum is the passageway that connects the colon to the anus.
- Sometimes abnormal growths, called polyps, form in the colon or rectum.
- Over time, some polyps may turn into cancer.
- Screening tests can find polyps so they can be removed before turning into cancer.
- Screening also helps find colorectal cancer at an early stage when treatment works best. (Colorectal Cancer – CDC)
Colorectal Cancer Videos
YouTube Videos that help explain types of Colon / Colorectal Cancer.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Colon / Colorectal Cancer
Treatments
Also see Treatments
Surgery (removing the cancer in an operation) is the most common treatment for all stages of colon cancer.
After the doctor removes all the cancer that can be seen at the time of the surgery, some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left. Treatment given after the surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
A doctor may remove the cancer using one of the following types of surgery:
- If the cancer is found at a very early stage, the doctor may remove it without cutting through the abdominal wall.
- Instead, the doctor may put a tube with a cutting tool through the rectum into the colon and cut the cancer out. This is called a local excision.
- If the cancer is found in a polyp (a small bulging area of tissue), the operation is called a polypectomy.
If the cancer is larger, the doctor will perform a partial colectomy (removing the cancer and a small amount of healthy tissue around it).
- The doctor may then perform an anastomosis (sewing the healthy parts of the colon together).
- The doctor will also usually remove lymph nodes near the colon and examine them under a microscope to see whether they contain cancer.
If the doctor is not able to sew the 2 ends of the colon back together, a stoma (an opening) is made on the outside of the body for waste to pass through. This procedure is called a colostomy.
- A bag is placed around the stoma to collect the waste.
- Sometimes the colostomy is needed only until the lower colon has healed, and then it can be reversed.
- If the doctor needs to remove the entire lower colon, however, the colostomy may be permanent.
- Radiofrequency ablation is the use of a special probe with tiny electrodes that kill cancer cells.
- Sometimes the probe is inserted directly through the skin and only local anesthesia is needed.
- In other cases, the probe is inserted through an incision in the abdomen. This is done in the hospital with general anesthesia.
Cryosurgery is a treatment that uses an instrument to freeze and destroy abnormal tissue. This type of treatment is also called cryotherapy.
Treatment for Stages of Colon Cancer
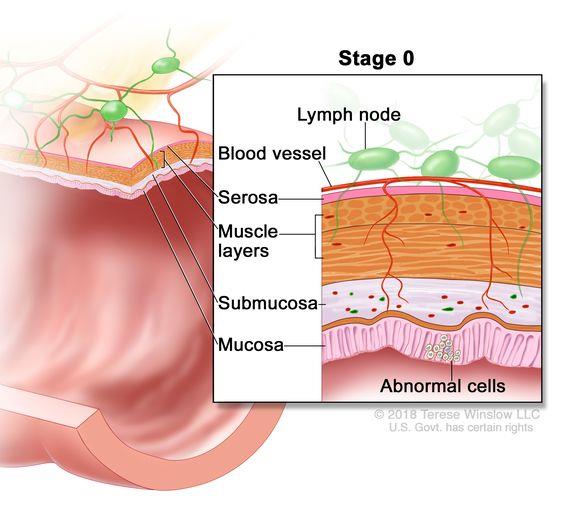
Abnormal cells are found in the mucosa (innermost layer) of the colon and/or rectal wall. These abnormal cells may become cancer and spread into nearby normal tissue.
Treatment of stage 0 (carcinoma in situ) may include the following types of surgery:
- Local excision or simple polypectomy.
- Local excision: The removal of tissue from the body using a scalpel (a sharp knife), laser, or other cutting tool. A surgical excision is usually done to remove a lump or other suspicious growth. Some normal tissue around the lump is usually removed at the same time.
- Simple polypectomy: Surgery to remove a polyp
- Resection and anastomosis. This is done when the tumor is too large to remove by local excision.
- Resection: Surgery to remove tissue or part or all of an organ.
- Anastomosis: A procedure to connect healthy sections of tubular structures in the body after the diseased portion has been surgically removed.
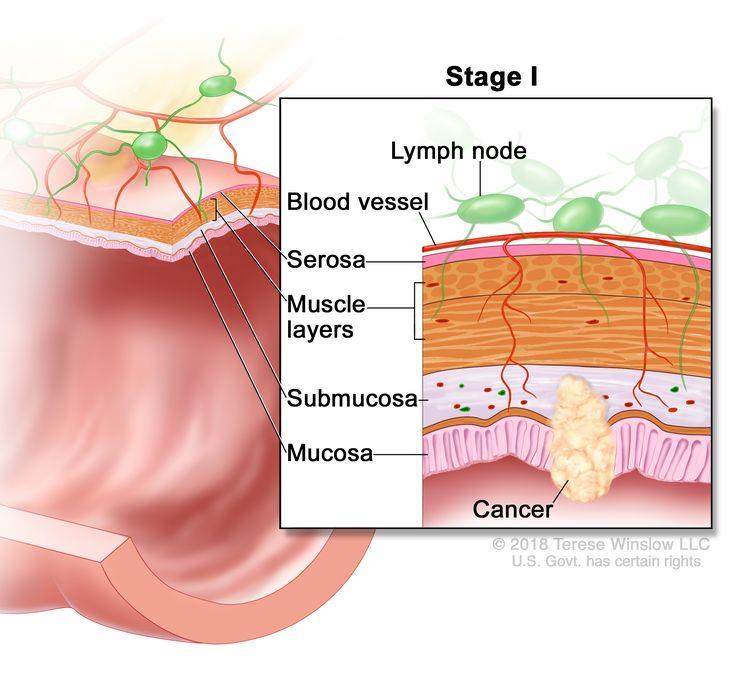
Cancer has formed in the mucosa (innermost layer) of the colon and/or rectum wall and has spread to the submucosa (layer of tissue next to the mucosa) or to the muscle layer of the colon and/or rectum wall.
- Also called Dukes A colorectal cancer.
Treatment of stage I colon cancer usually includes the following:
- Resection and anastomosis. This is done when the tumor is too large to remove by local excision.
- Resection: Surgery to remove tissue or part or all of an organ.
- Anastomosis: A procedure to connect healthy sections of tubular structures in the body after the diseased portion has been surgically removed.
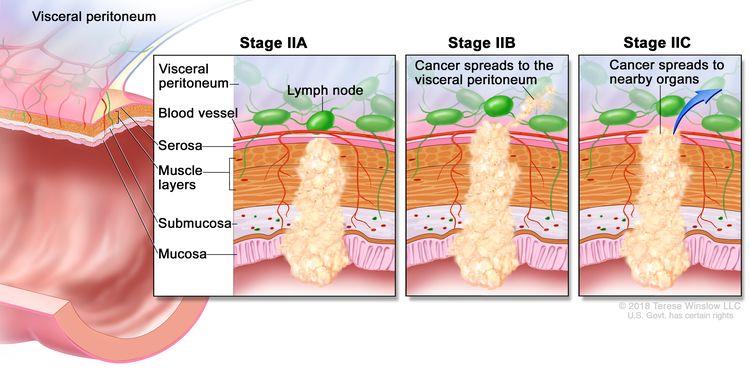
Stage II colorectal cancer is divided into stages IIA, IIB, and IIC.
- In stage IIA, cancer has spread through the muscle layer of the colon and/or rectum wall to the serosa (outermost layer) of the colon and/or rectum wall.
- In stage IIB, cancer has spread through the serosa of the colon and/or rectum wall to the tissue that lines the organs in the abdomen (visceral peritoneum).
- In stage IIC, cancer has spread through the serosa of the colon and/or rectum wall to nearby organs.
Treatment of stage II colon cancer may include the following:
- Resection and anastomosis. This is done when the tumor is too large to remove by local excision.
- Resection: Surgery to remove tissue or part or all of an organ.
- Anastomosis: A procedure to connect healthy sections of tubular structures in the body after the diseased portion has been surgically removed.
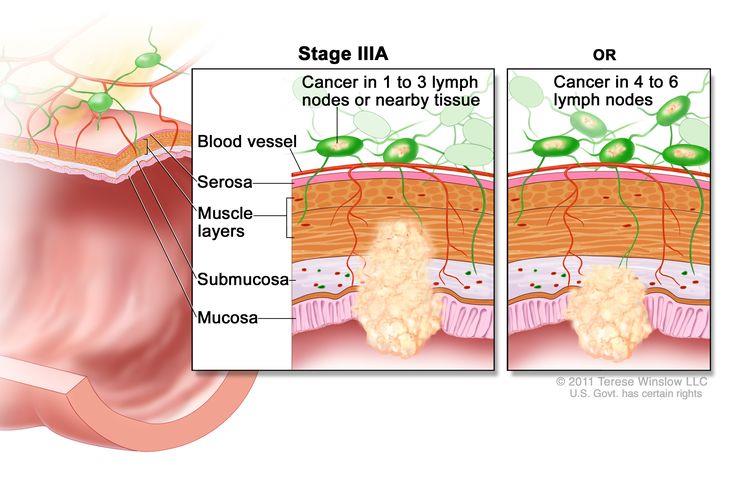
In stage IIIA, cancer has spread:
- Through the mucosa (innermost layer) of the colon wall to the submucosa (layer of tissue next to the mucosa) or to the muscle layer of the colon wall.
- Cancer has spread to one to three nearby lymph nodes or cancer cells have formed in tissue near the lymph nodes; or
- Through the mucosa (innermost layer) of the colon wall to the submucosa (layer of tissue next to the mucosa).
- Cancer has spread to four to six nearby lymph nodes.
Treatment of stage III colon cancer may include the following:
- Resection and anastomosis which may be followed by chemotherapy.
- Resection: Surgery to remove tissue or part or all of an organ.
- Anastomosis: A procedure to connect healthy sections of tubular structures in the body after the diseased portion has been surgically removed.
- Chemotherapy: Treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing.
- Chemotherapy may be given by mouth, injection, or infusion, or on the skin, depending on the type and stage of the cancer being treated.
- It may be given alone or with other treatments, such as surgery, radiation therapy, or biologic therapy.
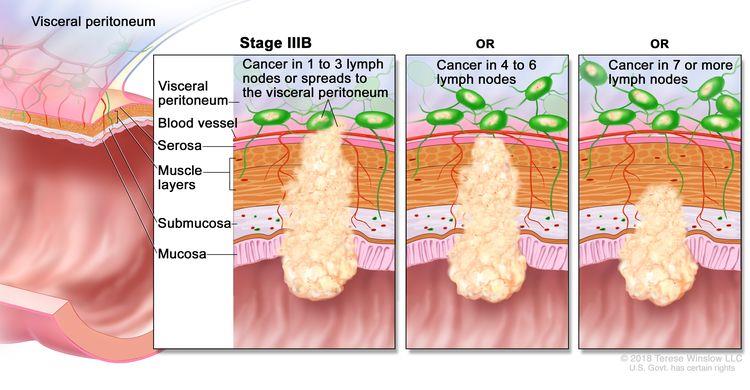
In stage IIIB, cancer has spread:
- Through the muscle layer of the colon wall to the serosa (outermost layer) of the colon wall or has spread through the serosa to the tissue that lines the organs in the abdomen (visceral peritoneum).
- Cancer has spread to one to three nearby lymph nodes or cancer cells have formed in tissue near the lymph nodes; or
- To the muscle layer or to the serosa (outermost layer) of the colon wall.
- Cancer has spread to four to six nearby lymph nodes; or
- Through the mucosa (innermost layer) of the colon wall to the submucosa (layer of tissue next to the mucosa) or to the muscle layer of the colon wall.
- Cancer has spread to seven or more nearby lymph nodes.
Treatment of stage III colon cancer may include the following:
- Resection and anastomosis which may be followed by chemotherapy.
- Resection: Surgery to remove tissue or part or all of an organ.
- Anastomosis: A procedure to connect healthy sections of tubular structures in the body after the diseased portion has been surgically removed.
- Chemotherapy: Treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing.
- Chemotherapy may be given by mouth, injection, or infusion, or on the skin, depending on the type and stage of the cancer being treated.
- It may be given alone or with other treatments, such as surgery, radiation therapy, or biologic therapy.
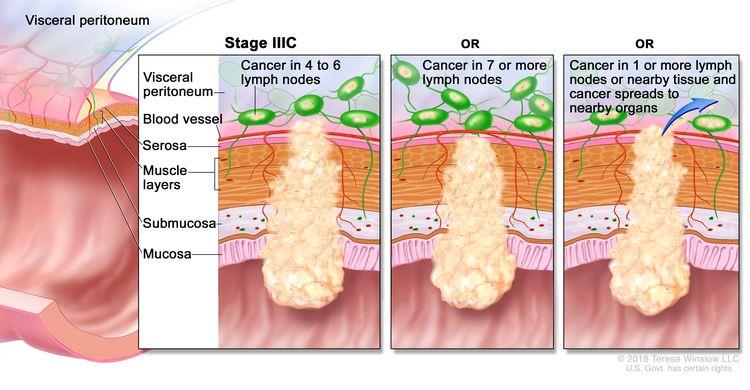
In stage IIIC, cancer has spread:
- Through the serosa (outermost layer) of the colon wall to the tissue that lines the organs in the abdomen (visceral peritoneum).
- Cancer has spread to four to six nearby lymph nodes; or
- Through the muscle layer of the colon wall to the serosa (outermost layer) of the colon wall or has spread through the serosa to the tissue that lines the organs in the abdomen (visceral peritoneum).
- Cancer has spread to seven or more nearby lymph nodes; or
- Through the serosa (outermost layer) of the colon wall to nearby organs.
- Cancer has spread to one or more nearby lymph nodes or cancer cells have formed in tissue near the lymph nodes.
Treatment of stage III colon cancer may include the following:
- Resection and anastomosis which may be followed by chemotherapy.
- Resection: Surgery to remove tissue or part or all of an organ.
- Anastomosis: A procedure to connect healthy sections of tubular structures in the body after the diseased portion has been surgically removed.
- Chemotherapy: Treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing.
- Chemotherapy may be given by mouth, injection, or infusion, or on the skin, depending on the type and stage of the cancer being treated.
- It may be given alone or with other treatments, such as surgery, radiation therapy, or biologic therapy.
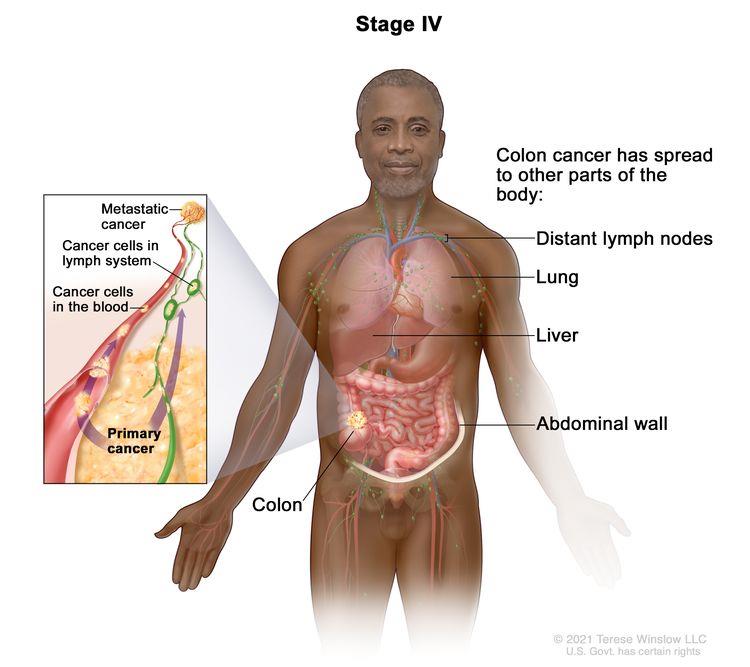
Stage IV colorectal cancer is divided into stages IVA, IVB, and IVC.
- In stage IVA, cancer has spread to one area or organ that is not near the colon and/or rectum, such as the liver, lung, ovary, or a distant lymph node.
- In stage IVB, cancer has spread to more than one area or organ that is not near the colon and/or rectum, such as the liver, lung, ovary, or a distant lymph node.
- In stage IVC, cancer has spread to the tissue that lines the wall of the abdomen and may have spread to other areas or organs.
Treatment of stage IV and recurrent colon cancer may include the following:
- Local excision for tumors that have recurred.
- Resection with or without anastomosis.
- Surgery to remove parts of other organs, such as the liver, lungs, and ovaries, where the cancer may have recurred or spread.
- Treatment of cancer that has spread to the liver may also include the following:
- Chemotherapy given before surgery to shrink the tumor, after surgery, or both before and after.
- Radiofrequency ablation or cryosurgery, for patients who cannot have surgery.
- Chemoembolization of the hepatic artery.
- Radiation therapy or chemotherapy may be offered to some patients as palliative therapy to relieve symptoms and improve quality of life.
- Chemotherapy and/or targeted therapy with a monoclonal antibody or an angiogenesis inhibitor.
- Targeted therapy with a protein kinase inhibitor and a monoclonal antibody in patients with a certain change in the BRAF gene.
- Immunotherapy.
- Clinical trials of chemotherapy and/or targeted therapy.
Risk Factors and Possible Side Effects
Your risk of getting colorectal cancer increases as you get older. Other risk factors include having:
- Inflammatory bowel disease such as Crohn’s disease or ulcerative colitis.
- A personal or family history of colorectal cancer or colorectal polyps.
- A genetic syndrome such as familial adenomatous polyposis (FAP)external icon or hereditary non-polyposis colorectal cancer (Lynch syndrome).
- Lifestyle factors that may contribute to an increased risk of colorectal cancer include—
- Lack of regular physical activity.
- A diet low in fruit and vegetables.
- A low-fiber and high-fat diet, or a diet high in processed meats.
- Overweight and obesity.
- Alcohol consumption.
- Tobacco use.
(Colorectal Cancer – CDC)
- Colostomy: attaches the end of your colon to an opening in your belly, where waste will leave your body. Some people only need to use a pouch while they heal from surgery. Once the colostomy is removed, you can use the bathroom normally again.
- Ileostomy: If there isn’t enough colon left, the end of your small intestine will be attached to the opening. You’ll wear a pouch on the outside of your body to collect waste.
- After surgery, you might be in some pain. Some people have bowel problems like constipation or diarrhea. These side effects often go away. It might take a few weeks or months for your bowel habits to get back to normal after surgery.
- If the tumor blocks your colon, the surgeon could put in a tube called a stent to keep the bowel open. You’ll get that stent put in during a colonoscopy.
(WebMD)
Recovery after Surgery
Information from CETI
Please follow MD/surgeon protocol, as every situation is unique.
Total Colectomy
Hospital Stay
Full Recovery
Restrictions
Exercise
Colectomy
Hospital Stay
Full Recovery
Restrictions
Exercise
Proctectomy
Hospital Stay
Full Recovery
Restrictions
Exercise
Low Anterior Resection
Hospital Stay
Full Recovery
Restrictions
Exercise
Abdominoperineal Resection
Hospital Stay
Full Recovery
Restrictions
Total Mesorectal Excision (TME)
Proctectomy with Colo-Anal Anastomosis
Hospital Stay
Full Recovery
Exercise
Pelvic Exenteration
Hospital Stay
Full Recovery
Restrictions
Exercise
Exercise after Surgery
Walking during recovery period for most patients – see MD protocol
- Avoid weightlifting or sits ups until cleared by MD
- Ostomy – Avoid contact sports and swimming – may need modifications. Avoid anything that causes intra-abdominal pressure or weightlifting due to risk of “blow” or hernia until cleared by MD
- Stoma – To avoid hernia, start with low resistance and progress slowly.
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
|
Information and pictures from National Cancer Institute unless otherwise specified |