Endometrial Cancer
Your Body is Your Temple
Research, Resources & Education
Table of Contents
Endometrial cancer is a serious condition that forms inside the uterus lining from multiplying endometrial cells. Factors that can contribute to its development are obesity, hormonal imbalances, age, family history, and medical conditions.
|
Information and pictures from National Cancer Institute unless otherwise specified |
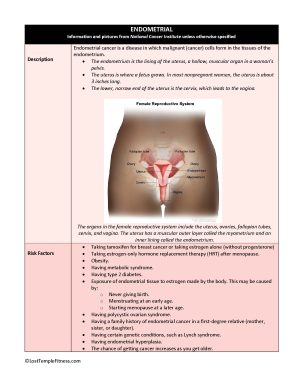
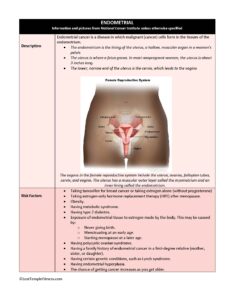
Endometrial Cancer Description
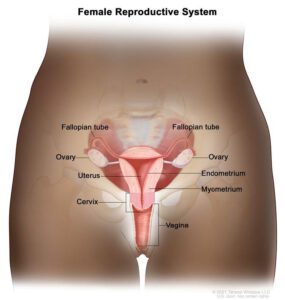
Endometrial cancer is a disease in which malignant (cancer) cells form in the tissues of the endometrium. • The endometrium is the lining of the uterus, a hollow, muscular organ in a woman’s pelvis.
- The uterus is where a fetus grows. In most nonpregnant women, the uterus is about 3 inches long.
- The lower, narrow end of the uterus is the cervix, which leads to the vagina.
The organs in the female reproductive system include the uterus, ovaries, fallopian tubes, cervix, and vagina. The uterus has a muscular outer layer called the myometrium and an inner lining called the endometrium.
Endometrial Cancer Videos
YouTube Videos that help explain Endometrial Cancer.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Endometrial /Uterine Cancer
Treatment for Endometrial Cancer
Also see Treatments
Surgery Surgery (removing the cancer in an operation) is the most common treatment for endometrial cancer. The following surgical procedures may be used:
- Total hysterectomy: Surgery to remove the uterus, including the cervix.
- If the uterus and cervix are taken out through the vagina, the operation is called a vaginal hysterectomy.
- If the uterus and cervix are taken out through a large incision (cut) in the abdomen, the operation is called a total abdominal hysterectomy.
- If the uterus and cervix are taken out through a small incision (cut) in the abdomen using a laparoscope, the operation is called a total laparoscopic hysterectomy.
- Bilateral salpingo-oophorectomy: Surgery to remove both ovaries and both fallopian tubes.
- Radical hysterectomy: Surgery to remove the uterus, cervix, and part of the vagina. The ovaries, fallopian tubes, or nearby lymph nodes may also be removed.
- Lymph node dissection: A surgical procedure in which the lymph nodes are removed from the pelvic area and a sample of tissue is checked under a microscope for signs of cancer. This procedure is also called lymphadenectomy.
After the doctor removes all the cancer that can be seen at the time of the surgery, some patients may be given radiation therapy or hormone treatment after surgery to kill any cancer cells that are left.
- Radiation therapy
- Targeted therapy
- Chemotherapy
- Hormone therapy
Risks and Possible Side Effects
Side Effect Information from Cancer Support Community
Risks
- Taking tamoxifen for breast cancer or taking estrogen alone (without progesterone)
- Taking estrogen-only hormone replacement therapy (HRT) after menopause.
- Obesity.
- Having metabolic syndrome.
- Having type 2 diabetes.
- Exposure of endometrial tissue to estrogen made by the body. This may be caused by:
- Never giving birth.
- Menstruating at an early age.
- Starting menopause at a later age.
- Having polycystic ovarian syndrome.
- Having a family history of endometrial cancer in a first-degree relative (mother, sister, or daughter).
- Having certain genetic conditions, such as Lynch syndrome.
- Having endometrial hyperplasia.
- The chance of getting cancer increases as you get older.
Possible Side Effects
Hysterectomy:
- Menstrual periods stop and can no longer get pregnant.
- Menopause starts immediately if ovaries are removed.
- Hot flashes and other symptoms of menopause may be worse than naturally occurring.
- May affect sexual intimacy.
Lymph Node Dissection:
- Lower extremity lymphedema (see Lymphedema section)
Radiation Therapy
- May include fatigue, nausea, vomiting, diarrhea, or other problems with digestion.
- Some women may have dryness, itching, tightening, and burning in the vagina.
- Doctors may advise their patients not to have intercourse during radiation therapy.
Hormonal Therapy Progesterone:
- May retain fluid, have an increased appetite, and gain weight.
- Women who are still menstruating may have changes in their periods.
Recovery after Surgery
Information from CETI
Please follow MD/surgeon protocol, as every situation is unique.
Laparoscopic Hysterectomy
Hospital Stay
Full Recovery
Restrictions
No intercourse for 8-12 weeks.
Exercise
Vaginal Hysterectomy
Hospital Stay
Full Recovery
Restrictions
No heavy lifting over 10 lbs.
Avoid sit ups, crunches, planks and high impact activities.
No intercourse for 8-12 weeks.
Exercise
Abdominal Hysterectomy
Hospital Stay
Full Recovery
Restrictions
No heavy lifting over 10 lbs.
Avoid sit ups, crunches, planks and high impact activities.
No intercourse for 8-12 weeks.
Exercise
Other Recommendations
- Exercise: Walk and stretch as soon as your doctor gives you the green light.
- Don’t lift anything heavier than 5-10 pounds for the full recovery period.
- Engage in abdominal exercises only after the full recovery period.
- Lower extremity lymphedema: May need to see lymphedema specialist. (See Lymphedema)
- Swelling of the abdomen is from fluid retention and abdominal gas and can last sometimes up to six months after the hysterectomy.
- Avoid the following until given the OK from MD
- High impact exercises such as running, jumping, burpees.
- High impact activities may also cause pelvic organ prolapse when the pelvic muscles have not been able to regain most of their pre- operative strength.
- Abdominal exercises such as sit ups, crunches, planks
- Heavily loaded resistance exercises requiring you to hold your breath or grunt to lift. This includes intense abdominal exertion, stretching or putting extra pressure on the pelvic floor for at least 6 to 8 weeks after your surgery.
- Heavy lifting will increase the pressure in the abdominal area and put extra tension on the healing wound.
Examples of Exercise or Stretches after Hysterectomy
Please follow MD/surgeon protocol, as every situation is unique.
- Start by lying on your back, with knees bent and feet flat. Take a gentle inhale breath for 3-4 seconds, breathing into your ribcage and tummy, and gently exhale through pursed lips for 5 seconds.
- Think of your pelvic floor like an elevator, with closing doors and a G floor, and 1st floor.
- Start your pelvic floor contraction by ‘closing the elevator doors’ (squeeze around anus and urethra like you are trying to stop the flow of urine)
- Then, feel a gentle lift of the pelvic floor elevator up to the 1st floor.
- Get on your hands and knees.
- Position your shoulders right above your hands and your hips above the knees.
- While you take a deep breath, you let your belly hang to the ground. Next, you exhale and pull your stomach in as far as you can.
- Hold this position for 10 seconds and relax for 5 seconds. you can start with 6 to 8 repetitions.
- Lie down with your knees bent and your arms crossed over your stomach or folded in back of your head.
- Use your hands to gently pull your abdominal muscles together and raise your head and point your chin toward your chest.
- Hold the position for 3 to 5 seconds and slowly return your head to the starting position.
- Relax and repeat the movement.
Take long, slow breaths, completely filling the lungs, belly and rib cage before slowly exhaling.
See Kegel under Bladder section
If lymph nodes were removed or had radiation, please see lymphedema section.
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
|
Information and pictures from National Cancer Institute unless otherwise specified |