Lymphedema Prevention,
Treatment & Exercise
Your Body is Your Temple
Research, Resources & Education
Table of Contents
Hints to prevent lymphedema and treatments such as skin care, manual lymph drainage, bandaging, compression, exercise & pressure garments. Axillary Reverse Mapping. Exercise is important in promoting lymph drainage.
Information and pictures from National Cancer Institute unless otherwise specified
Lymphedema Self Care Videos
YouTube Videos that help explain types of treatment including dry brushing, lymph drainage and bandaging.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Find other lymphedema self care videos not provided on YourTube by Klose Education including Head & Neck.
Lymphedema Self Care
Self Manual Lymph Drainage
Self Bandaging
Complete Decongestive Therapy
- Combined physical therapy or complete decongestive therapy is a program managed by a certified lymphedema therapist to include:
- Manual lymphatic drainage
- Compression bandaging
- Exercise
- Skin care
- Patient education
- At the beginning of the program, the therapist gives many treatments over a short time to decrease most of the swelling in the limb with lymphedema.
- The patient then continues the program at home to keep the swelling down.
Preventative Measures
Keep skin and nails clean and cared for, to prevent infection.
- Bacteria can enter the body through a cut, scratch, insect bite, or other skin injury.
- Fluid that is trapped in body tissues by lymphedema makes it easy for bacteria to grow and cause infection.
- Look for signs of infection, such as redness, pain, swelling, heat, fever, or red streaks below the surface of the skin.
- Call your doctor right away if any of these signs appear.
Careful skin and nail care helps prevent infection:
- Use cream or lotion to keep the skin moist.
- Treat small cuts or breaks in the skin with an antibacterial ointment.
- Avoid needle sticks of any type into the limb (arm or leg) with lymphedema.
- This includes shots or blood tests.
- Use a thimble for sewing.
- Avoid testing bath or cooking water using the limb with lymphedema.
- There may be less feeling (touch, temperature, pain) in the affected arm or leg, and skin might burn in water that is too hot.
- Wear gloves when gardening and cooking.
- Wear sunscreen and shoes when outdoors.
- Cut toenails straight across.
- See a podiatrist (foot doctor) as needed to prevent ingrown nails and infections.
- Keep feet clean and dry and wear cotton socks.
Avoid blocking the flow of fluids through the body.
- It is important to keep body fluids moving, especially through an affected limb or in areas where lymphedema may develop.
- Do not cross legs while sitting.
- Change sitting position at least every 30 minutes.
- Wear only loose jewelry and clothes without tight bands or elastic.
- Do not carry handbags on the arm with lymphedema.
- Do not use a blood pressure cuff on the arm with lymphedema.
- Do not use elastic bandages or stockings with tight bands.
Keep blood from pooling in the affected limb.
- Keep the limb with lymphedema raised higher than the heart when possible.
- Do not swing the limb quickly in circles or let the limb hang down.
- This makes blood and fluid collect in the lower part of the arm or leg.
- Do not apply heat to the limb.
Treatments
Information from National Cancer Institute (NIH) and Klose Education & Training
|
MLD (manual therapy) for lymphedema should begin with someone specially trained in treating lymphedema.
- In this type of massage, the soft tissues of the body are lightly rubbed, tapped, and stroked.
- It is a very light touch, almost like a brushing.
- MLD may help move lymph out of the swollen area into an area with working lymph vessels.
- Patients can be taught to do this type of massage therapy themselves by a certified lymphatic therapist. (NCI)
Effects:
- Increases reabsorption of protein rich fluid
- Increases lymphatic activity
- Promotes relaxation
- Creates and analgesic effect (Klose Education)
When done correctly, massage therapy does not cause medical problems.
- Massage should not be done on any of the following:
- Open wounds, bruises, or areas of broken skin.
- Tumors that can be seen on the skin surface.
- Areas with deep vein thrombosis (blood clot in a vein).
- Sensitive soft tissue where the skin was treated with radiation therapy. (NCI)
Contraindications:
- Acute infections, such as cellulitis
- Untreated congestive heart failure (CHF)
- Malignant disease – cancer
- Renal dysfunction
- Acute undiagnosed DVT (Klose Education)
- Once the lymph fluid is moved out of a swollen limb, bandaging (wrapping) can help prevent the area from refilling with fluid.
- Bandages also increase the ability of the lymph vessels to move lymph along.
- Lymphedema that has not improved with other treatments is sometimes helped with bandaging. (NIH)
INDICATIONS:
- Lymphedema
- Chronic venous insufficiency (CVI )
- Combination venous and lymphatic edema
- Lipedema
- Post‐traumatic edema
- Post‐surgical edema
- Acute DVT (with physician dx)
CONTRAINDICATION:
- Acute infections (MD must clear patient)
- Arterial wounds
- Arterial disease (ABI 0.8 or below)
- Acute DVT (without physician dx)
- Cardiac edema (untreated CHF)
- Acute trauma without diagnosis
PRECAUTIONS:
- Sensory deficits
- Malignancy
- Diabetes – Small vessel (arteriole) and sensory deficits
- Toe bandaging may be contraindicated
- Paralysis
- Poor cognition or altered mental status
- Sensitivity to the products used for bandaging (Klose Education)
Pressure garments are made of fabric that puts a controlled amount of pressure on different parts of the arm or leg to help move fluid and keep it from building up.
- Some patients may need to have these garments custom-made for a correct fit.
- Wearing a pressure garment during exercise may help prevent more swelling in an affected limb.
- It is important to use pressure garments during air travel, because lymphedema can become worse at high altitudes.
- Pressure garments are also called compression sleeves and lymphedema sleeves or stockings. (NIH)
Compression devices are pumps connected to a sleeve that wraps around the arm or leg and applies pressure on and off.
- The sleeve is inflated and deflated on a timed cycle.
- This pumping action may help move fluid through lymph vessels and veins and keep fluid from building up in the arm or leg.
- Compression devices may be helpful when added to complete decongestive therapy.
- The use of these devices should be supervised by a trained professional because too much pressure can damage lymph vessels near the surface of the skin. (NIH)
Weight loss
- In patients who are overweight, lymphedema related to breast cancer may improve with weight loss.
Laser therapy
- Laser therapy may help decrease lymphedema swelling and skin hardness after a mastectomy.
- A hand-held, battery-powered device is used to aim low-level laser beams at the area with lymphedema.
Drug therapy
- Lymphedema is not usually treated with drugs.
- Antibiotics may be used to treat and prevent infections.
- Other types of drugs, such as diuretics or anticoagulants (blood thinners), is usually not helpful and may make the lymphedema worse.
Surgery
- Lymphedema caused by cancer is rarely treated with surgery. NIH
The axillary reverse mapping (ARM) technique has been developed to map and preserve arm lymphatic drainage during ALND and/or SLNB, thereby minimizing arm lymphedema.
- However, the success of ARM in reducing lymphedema has not been exactly determined.
- If ARM can be confirmed to be both effective and oncologically safe in preventing lymphedema, this technique should be recommended in the management of breast cancer treatment. (NIH) – National Library of Medicine.
Axillary Reverse Mapping (ARM): Where to Go
- Lymphedema is a major chronic morbidity that occurs in patients undergoing treatment for breast cancer (BC). Surgery for BC includes axillary surgery with either sentinel lymph node biopsy (SLNB) or axillary lymph node dissection (ALND).
- Lymphedema occurs due to removal or disruption of lymphatic drainage of the arm that overlaps with drainage of the breast.
- The risk of lymphedema increases significantly with adjuvant radiation.
- Axillary reverse mapping (ARM) is a technique where blue dye is injected into the upper arm at surgery, allowing direct visualization of arm lymphatics and nodes during either SLNB or ALND.
- This allows preservation of arm lymphatics unless there is suspicion of metastatic disease in ARM lymphatics or if the ARM node is/are also the sentinel lymph node.
- Studies to date have largely been observational cohort studies, and mainly with low risk patients undergoing SLNB only.
- There is only one published randomized controlled trial, and this included only patients undergoing modified radical mastectomy.
- (NIH) – National Library of Medicine.
Axillary Reverse Mapping (ARM) Technique (ARM)
- Traditionally, the rates of arm swelling after sentinel node biopsy range from 3‐8%1 and from 13‐40%2 after axillary dissection surgery.
- The studies that looked at ARM show a lymphedema rate that is lower, around 1‐3% for the sentinel node surgery and 4‐9%3 for the axillary dissection surgery.
- Sometimes, it is not always possible to do ARM, and the surgeon needs to inject the blue dye in the breast to help identify the correct lymph nodes.
- This may be the case if you have had previous chemotherapy in the breast, or if the lymph nodes are not accurately found with other methods.
- Additionally, it is possible that the blue lymph nodes and the channels that are identified to drain the arm need to be removed to treat your cancer safely.
- If this is the case, you may be placed in a special group to watch your arm swelling closely, or even have the option of having these channels reconnected.
- This is usually done by surgeons well experienced in lymphatic surgery, and may include plastic surgeons also. Summit Education: Oncology Rehab Dec 12, 2019
Exercise
Both light exercise and aerobic exercise (physical activity that causes the heart and lungs to work harder) help the lymph vessels move lymph out of the affected limb and decrease swelling.
- Talk with a certified lymphedema therapist before beginning exercise.
- Patients who have lymphedema or who are at risk for lymphedema should talk with a certified lymphedema therapist before beginning an exercise routine.
- (See the Lymphology Association of North America web site for a list of certified lymphedema therapists in the US)
- Wear a pressure garment if lymphedema has developed.
- Patients who have lymphedema should always wear a well-fitting pressure garment during all exercise that uses the affected limb or body part.
- When it is not known for sure if a woman has lymphedema, upper-body exercise without a garment may be more helpful than no exercise at all.
- Patients who do not have lymphedema do not need to wear a pressure garment during exercise.
- Breast cancer survivors should begin with light upper-body exercise and increase it slowly.
- Some studies with breast cancer survivors show that upper-body exercise is safe in women who have lymphedema or who are at risk for lymphedema.
- Weight-lifting that is slowly increased may keep lymphedema from getting worse.
- Exercise should start at a very low level, increase slowly over time, and be overseen by the lymphedema therapist.
- If exercise is stopped for a week or longer, it should be started again at a low level and increased slowly.
- If symptoms (such as swelling or heaviness in the limb) change or increase for a week or longer, talk with the lymphedema therapist.
- It is likely that exercising at a low level and slowly increasing it again over time is better for the affected limb than stopping the exercise completely.
- More studies are needed to find out if weight-lifting is safe for cancer survivors with lymphedema in the legs. (NIH)
Upper & Lower Extremity Exercises and Breathing
Upper Extremity Exercises

Fist Clench
Lymphedema control and circulation
Hands on thighs, open and close hand

Fist Clench
Lymphedema control and circulation
Open and close your hand 15-20x with arm elevated above heart to prevent edema
NOT OVERHEAD first 1-2 weeks and/or until drains are out

Fist Clench
Lymphedema control and circulation
Open and close your hand 15-20x with arm elevated above heart to prevent edema

Shoulder Rolls - Backwards
Move your shoulders in a circular pattern so that your are moving in an up, back and down direction.
Perform small circles if needed for comfort.

Shrugs
Raise your shoulders upward towards your ears as shown.
Shrug both shoulders at the same time.
Inhale up/exhale down

Neck Rotation and Side Bends
SIDE BENDS: (Top) Tilt your head as if you are trying to touch your ear to your shoulder.
ROTATION: (Bottom) Turn you head to the side as if looking over your shoulder.
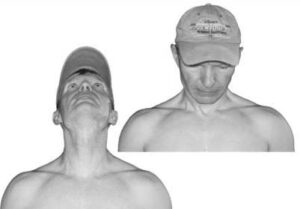
Neck Extension & Flexion
EXTENSION: Look up as if you are looking at the sky moving your neck only.
FLEXION: Look down as if you are looking at the floor.
For an extra stretch gentely put both hands behind your head to move chin towards the chest and hold.
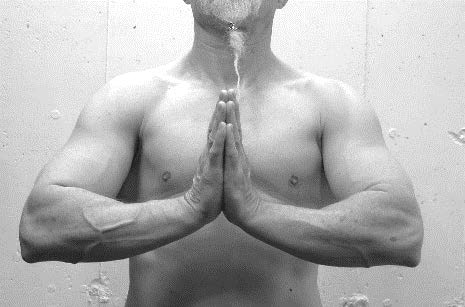
Isometric Chest Press
Place the palms of your hands together with your elbows bent and arms at shoulder level or below.
Exhale while pushing hands together and inhale and relax. 5-10x.

Shoulder Raise / Elbow Circles
Place your fingertips onto your shoulders.
Slowly raise the elbow up to the side, then move it forwards, gently circling your arm.
You are aiming to get your elbow level with your shoulder.
Try to increase the height each time you do the exercises until you get level with your shoulder.
Lower Extremity Exercises

Ankle Plantar & Dorsi Flexion - Circles
Lymphedema control and circulation
Lying on your back, extend the legs towards the ceiling.
- Dorsi/plantar flex foot (ankle pump) ~10x.
- Foot circles ~10x each direction

Leg Circle
Lymphedema control and circulation
Lying on your back, bend one leg and point the opposite leg towards the ceiling.
Move the leg in a small circumduction ~10x each way. Think of drawing a small circle on the ceiling with your foot.
Repeat on the opposite leg.

Leg Flexion & Extension
Lymphedema control and circulation
Lying on your back, bend and extend leg ~10x repetitions.
You can either alternate or repeat on the same leg and repeat with opposite leg.

Bicycles
Lymphedema control and circulation
Lying on your back, bend the knees at an angle.
In a circular motion, complete ~10 repetitions in each direction, as if on a bike
Diaphragmatic Breathing

Diaphragmatic Breathing
Lie either on your back with your knees bent or sit up
Inhale through your nose; as you do so, allow your stomach to rise.
Limit movement in your chest.
Attempt to push your bottom ribs out to the side as you breathe in.
Exhale through your mouth; as you do so, allow your stomach to fall. Limit movement in your chest.
Diaphragmatic breathing 6x a day for 5-10 repetitions
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
|
Information and pictures from National Cancer Institute unless otherwise specified |