Mastectomy:
Tissue Flap Surgery vs. Implants
Your Body is Your Temple
Research, Resources & Education
Table of Contents
Implants can be inserted underneath the skin or chest muscle following the mastectomy to help build a breast-like shape.
Another option is tissue flap surgery, which is suitable for women who lack tissue for implants or prefer a natural-looking result. Tissue flap surgery is a specialized procedure that creates a new breast shape using muscle, fat, and skin from other parts of the patient's body.
Information and pictures from National Cancer Institute unless otherwise specified
Videos - Tissue Flap / Autologous Tissue Surgeries
YouTube Videos that help explain different types of Breast Tissue Flap Surgery & Nipple Reconstruction Options.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Tissue Flap & Nipple Reconstruction
Tissue Flap Surgery / Autologous Tissue & Reconstruction
Tissue Flap Surgery
In tissue flap surgery, a reconstructive plastic surgeon builds a new breast-like shape from muscle, fat, and skin taken from other parts of your body (usually your belly, back, or buttock).
- This new breast-like shape should last the rest of your life.
- Women who are very thin or obese, smoke, or have serious health problems often cannot have tissue flap surgery.
- Healing after tissue flap surgery often takes longer than healing after breast implant surgery.
- You may have other problems, as well. For example, if you have a muscle removed, you might lose strength in the area from which it was taken.
- You may get an infection or have trouble healing.
- Tissue flap surgery is best done by a reconstructive plastic surgeon who has special training in this type of surgery and has done it many times before.
Autologous Tissue
In autologous tissue reconstruction, a piece of tissue containing skin, fat, blood vessels, and sometimes muscle is taken from elsewhere in a woman’s body and used to rebuild the breast.
- This piece of tissue is called a flap.
- Different sites in the body can provide flaps for breast reconstruction.
- Flaps used for breast reconstruction most often come from the abdomen or back.
- However, they can also be taken from the thigh or buttocks.
Depending on their source, flaps can be pedicled or free.
- With a pedicled flap, the tissue and attached blood vessels are moved together through the body to the breast area.
- Because the blood supply to the tissue used for reconstruction is left intact, blood vessels do not need to be reconnected once the tissue is moved.
- With free flaps, the tissue is cut free from its blood supply.
- It must be attached to new blood vessels in the breast area, using a technique called microsurgery.
- This gives the reconstructed breast a blood supply.
- Flaps taken from the thigh or buttocks are used for women who have had previous major abdominal surgery or who don’t have enough abdominal tissue to reconstruct a breast.
- These types of flaps are free flaps.
- With these flaps an implant is often used as well to provide sufficient breast volume.
- In some cases, an implant and autologous tissue are used together.
- For example, autologous tissue may be used to cover an implant when there isn’t enough skin and muscle left after mastectomy to allow for expansion and use of an implant.
Reconstruction with Autologous Tissue
Surgery and recovery
- Longer surgical procedure than for implants
- The initial recovery period may be longer than for implants
- Pedicled flap reconstruction is usually a shorter operation than free flap reconstruction and usually requires a shorter hospitalization
- Free flap reconstruction is a longer, highly technical operation compared with pedicled flap reconstruction that requires a surgeon who has experience with microsurgery to re-attach blood vessels
Possible complications
- Necrosis (death) of the transferred tissue
- Blood clots may be more frequent with some flap sources
- Pain and weakness at the site from which the donor tissue was taken
- Obesity, diabetes, and smoking may increase the rate of complications
Other considerations
- May provide a more natural breast shape than implants
- May feel softer and more natural to the touch than implants
- Leaves a scar at the site from which the donor tissue was taken
- Can be used to replace tissue that has been damaged by radiation therapy
- All women who undergo mastectomy for breast cancer experience varying degrees of breast numbness and loss of sensation (feeling) because nerves that provide sensation to the breast are cut when breast tissue is removed during surgery.
- However, a woman may regain some sensation as the severed nerves grow and regenerate, and breast surgeons continue to make technical advances that can spare or repair damage to nerves.
- Any type of breast reconstruction can fail if healing does not occur properly.
- In these cases, the implant or flap will have to be removed.
- If an implant reconstruction fails, a woman can usually have a second reconstruction using an alternative approach.
Information and pictures in the following section from the
Mayo Clinic – Breast reconstruction with flap surgery unless otherwise specified
Abdomen: TRAM Flap
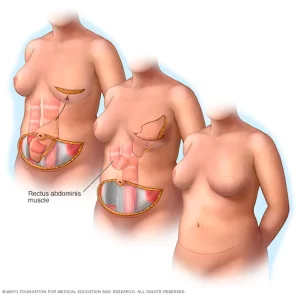
Tissue comes from the lower abdomen as in a DIEP flap but includes muscle. It can be
either pedicled or free. (NIH)
- Your surgeon removes tissue — including muscle — from your abdomen in a procedure known as a transverse rectus abdominis muscle (TRAM) flap.
- The TRAM flap can be transferred as a free flap or a pedicled flap.
- A pedicled TRAM flap uses your whole rectus muscle — one of the four major muscles in your abdomen.
- For a muscle-sparing free TRAM flap, your surgeon takes only a portion of your rectus abdominis muscle, which may help you retain abdominal strength after surgery.
Pedicled Tram Flap (top) and Free TRAM Flap (bottom)
(Mayo)
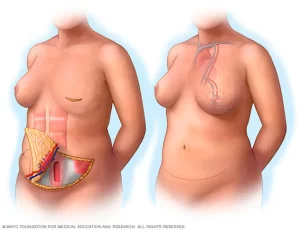
Abdomen: DIEP Flap
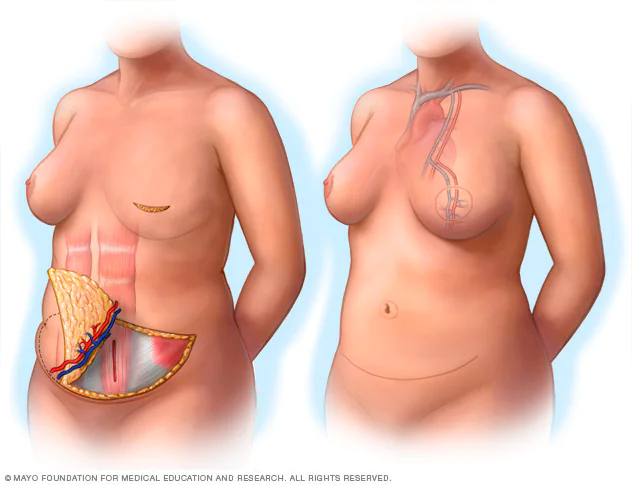
Tissue comes from the abdomen and contains only skin, blood vessels, and fat, without the underlying muscle. This type of flap is a free flap. (NCI)
- A newer procedure, deep inferior epigastric perforator (DIEP) flap, is similar to a TRAM flap, but only skin and fat are removed.
- Most of the abdominal muscle is left in place and minimal muscle tissue is taken to form the new breast mound.
- Reattaching blood vessels requires expertise in surgery through a microscope (microsurgery).
- An advantage to this type of breast reconstruction is that you’ll retain more strength in your abdomen.
- If your surgeon can’t perform a DIEP flap procedure for anatomical reasons, he or she might opt for the TRAM procedure instead.
DIEP flap – Pictures from Mayo Clinic
Abdomen: SIEA Flap - AKA SIEP Flap
Tissue comes from the abdomen as in a DIEP flap but includes a different set of blood vessels.
- It also does not involve cutting of the abdominal muscle and is a free flap.
- This type of flap is not an option for many women, as the necessary blood vessels are not adequate or do not exist. (NCI)
- A variation of the DIEP flap, the superficial inferior epigastric artery (SIEA) flap uses the same abdominal tissue but relies on blood vessels that aren’t as deep within the abdomen.
- This provides a less invasive option, but not all women’s SIEA blood vessels are adequate for this type of flap surgery. (Mayo Clinic.org)
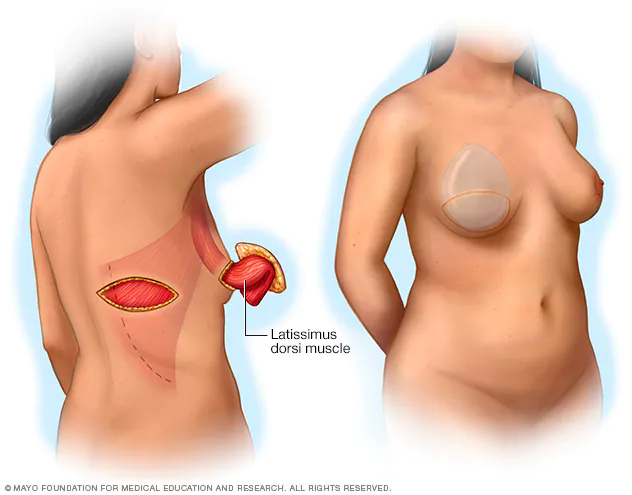
Back: Latissimus dorsi Flap (LAT flap)
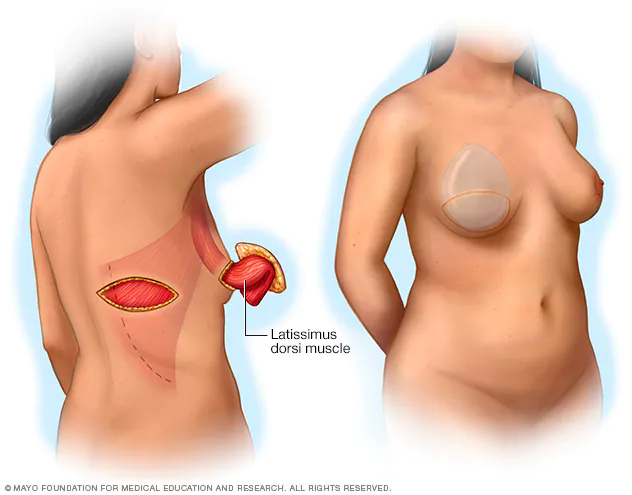
Tissue comes from the middle and side of the back.
- This type of flap is pedicled when used for breast reconstruction. (LD flaps can be used for other types of reconstruction as well.) (NCI)
- This surgical technique takes skin, fat and muscle from your upper back, tunneling it under your skin to your chest.
- Because the amount of skin and other tissue is generally less than in a TRAM flap surgery, this approach may be used for small and medium-sized breasts or for creating a pocket for a breast implant.
- Although uncommon, some women experience muscle weakness in the back, shoulder or arm after this surgery.
Latissimus dorsi (LD) flap – Mayo Clinic
Buttock (gluteal) Flap
A gluteal flap is a free flap procedure that takes tissue from your buttocks and transplants it to your chest area.
- A gluteal flap may be an option for women who prefer tissue reconstruction but who don’t have enough extra tissue in their backs or abdomens. (Mayo Clinic.org)
PAP flap: Tissue, without muscle, that comes from the upper inner thigh.
SGAP flap: Tissue comes from the buttocks as in an IGAP flap, but includes a different set of blood vessels and contains only skin, blood vessels, and fat. (NCI)
Thigh Flaps (TUG) & (IGAP)
Inner thigh (TUG). Another newer option, the transverse upper gracilis (TUG) flap, uses muscle and fatty tissue from the bottom of the buttocks to the inner thigh.
- TUG flap surgery, which isn’t available everywhere, may be an option for women whose thighs touch and who have small to medium-sized breasts. (Mayo Clinic.org)
IGAP flap: Tissue comes from the buttocks and contains only skin, blood vessels, and fat.
TUG flap: Tissue, including muscle that comes from the upper inner thigh. (NCI)
Nipple Reconstruction
Tissue comes from the middle and side of the back.
- This type of flap is pedicled when used for breast reconstruction. (LD flaps can be used for other types of reconstruction as well.) (NCI)
- This surgical technique takes skin, fat and muscle from your upper back, tunneling it under your skin to your chest.
- Because the amount of skin and other tissue is generally less than in a TRAM flap surgery, this approach may be used for small and medium-sized breasts or for creating a pocket for a breast implant.
- Although uncommon, some women experience muscle weakness in the back, shoulder or arm after this surgery.
Latissimus dorsi (LD) flap – Mayo Clinic
Videos - Breast Implants & Tissue Expanders
YouTube Videos that help explain different types of Breast, Implants& Tissue Expanders.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Breast Implants & Tissue Expanders
Breast Implants & Tissue Expanders
Information from National Cancer Institute or John Hopkins Medicine unless otherwise specified

Breast Implant
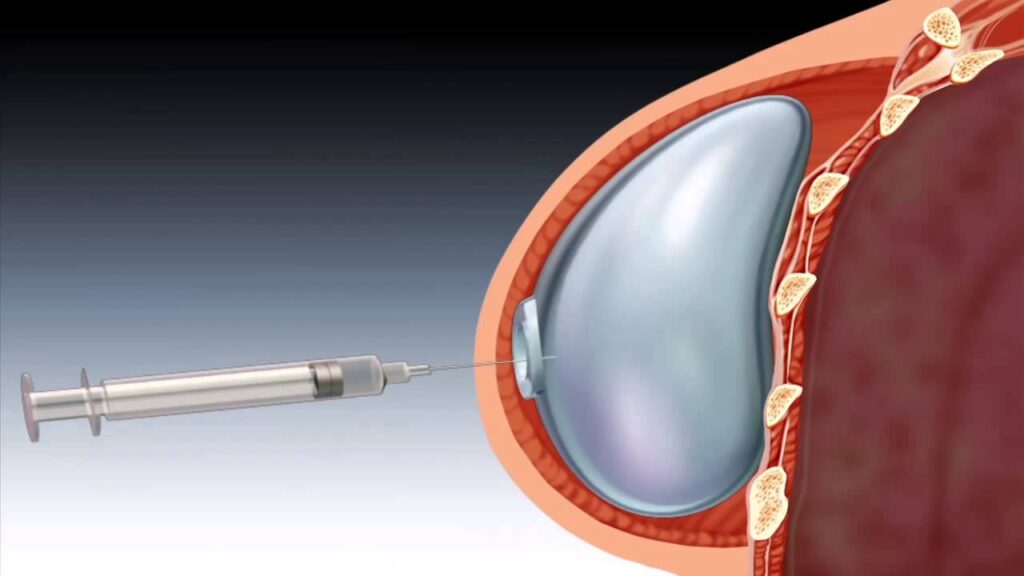
Implants are inserted underneath the skin or chest muscle following the mastectomy.
- (Most mastectomies are performed using a technique called skin-sparing mastectomy, in which much of the breast skin is saved for use in reconstructing the breast.) Implants are usually placed in two parts:
- The first step is called tissue expansion.
- This is when the plastic surgeon places a balloon expander under the chest muscle (usually over the pectoralis minor and under the pectoralis major).
- Over many weeks, saline (salt water) will be added to the expander to stretch the chest muscle and the skin on top of it by the plastic surgeon.
- This process makes a pocket for the implant.
- After the chest tissue has relaxed and healed enough, the expander is removed and replaced with an implant (filled with saline or silicone gel).
- The chest tissue is usually ready for the implant 2 to 6 months after mastectomy.
- This creates a new breast-like shape. Although this shape looks like a breast, you will not have the same feeling in it because nerves were cut during your mastectomy.
- In some cases, the implant can be placed in the breast during the same surgery as the mastectomy—that is, a tissue expander is not used to prepare for the implant.
- Surgeons are increasingly using material called acellular dermal matrix as a kind of scaffold or “sling” to support tissue expanders and implants.
- Acellular dermal matrix is a kind of mesh that is made from donated human or pig skin that has been sterilized and processed to remove all cells to eliminate the risks of rejection and infection.
- Breast implants do not last a lifetime. If you choose to have an implant, chances are you will need more surgery later on to remove or replace it.
- Implants can cause problems such as breast hardness, pain, and infection.
- The implant may also break, move, or shift.
- These problems can happen soon after surgery or years later.
- Chemotherapy or radiation may be recommended to you by your surgical oncologist following your mastectomy.
- If you choose to have these treatments it will delay the tissue expansion process by approximately four to eight weeks. (John Hopkins Medicine – Tissue Expanders)
(NCI)
Tissue Expanders
Tissue expansion involves expansion of the breast skin and muscle using a temporary tissue expander.
- A few months later, the expander is removed and the patient receives either microvascular flap reconstruction, or the insertion of a permanent breast implant.
- This type of breast reconstruction requires two separate operations.
What is a breast tissue expander?
- A breast tissue expander is an inflatable breast implant designed to stretch the skin and muscle to make room for a future, more permanent implant.
- At the same time your mastectomy is done by our breast surgical oncologist, the breast plastic and reconstructive surgeon will insert a tissue expander beneath your skin and chest muscle.
- Through a tiny valve mechanism located inside the expander, the nurse practitioner will periodically inject a salt-water solution to gradually fill the expander over several weeks or months.
- You may feel a sensation of stretching and pressure in the breast area during this procedure, but most women find it is not too uncomfortable.
- This process will usually begin three to four weeks after your mastectomy, once your drains are removed, and will continue until the size is slightly larger than your other breast.
- After the skin over the breast area has stretched enough, the expander will be removed in a second operation and either flap reconstruction or a permanent implant will be inserted.
- The nipple and the dark skin surrounding it, called the areola, are reconstructed in a subsequent procedure. (John Hopkins Medicine – Tissue Expanders)
- Expanders could be in for up to a year or more if chemotherapy and radiation are done after surgery.
- Implants are placed 3-6 weeks after chemotherapy is complete or 6 months after radiation.
Common Side Effects:
- Pain and Stiffness
- Often numb at fill site
- Difficult to lie on side
- Postural changes
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
Information and pictures from National Cancer Institute unless otherwise specified