Pancreatic Cancer
Your Body is Your Temple
Research, Resources & Education
Table of Contents
Pancreatic cancer is a serious disease affecting the pancreas. It causes abnormal cell growth leading to tumors that can be benign or malignant. The malignant tumors spread to other parts of the body if not treated. Diagnosis is difficult due to non-specific symptoms.
Information and pictures from National Cancer Institute unless otherwise specified
Pancreas Anatomy and Purpose
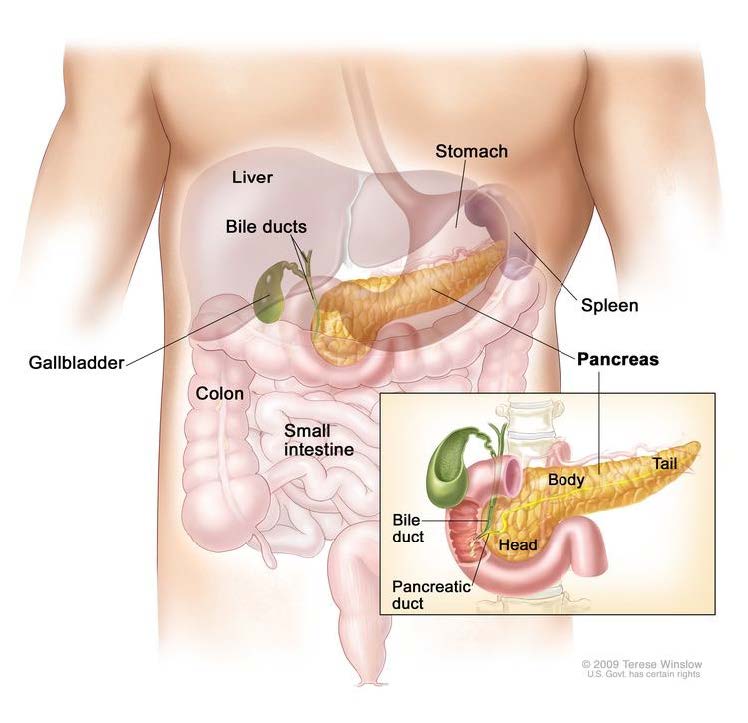
The pancreas is a gland about 6 inches long that is shaped like a thin pear lying on its side.
- The wider end of the pancreas is called the head, the middle section is called the body, and the narrow end is called the tail.
- The pancreas lies between the stomach and the spine.
- The pancreas has three areas: head, body, and tail.
- It is found in the abdomen near the stomach, intestines, and other organs.
The pancreas has two main jobs in the body:
- To make juices that help digest (break down) food.
- The digestive juices are made by exocrine
- To make hormones, such as insulin and glucagon, that help control blood sugar levels.
- Both of these hormones help the body use and store the energy it gets from food
Pancreatic Cancer Videos
YouTube Videos that help explain Pancreatic Cancer.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Pancreatic Cancer
Treatments
Also see Treatments
One of the following types of surgery may be used to take out the tumor:
- Whipple procedure: A surgical procedure in which the head of the pancreas, the gallbladder, part of the stomach, part of the small intestine, and the bile duct are removed.
- Enough of the pancreas is left to produce digestive juices and insulin.
- Total pancreatectomy: This operation removes the whole pancreas, part of the stomach, part of the small intestine, the common bile duct, the gallbladder, the spleen, and nearby lymph nodes.
- Distal pancreatectomy: Surgery to remove the body and the tail of the pancreas.
- The spleen may also be removed if cancer has spread to the spleen.
If the cancer has spread and cannot be removed, the following types of palliative surgery may be done to relieve symptoms and improve quality of life:
- Biliary bypass: If cancer is blocking the bile duct and bile is building up in the gallbladder, a biliary bypass may be done.
- During this operation, the doctor will cut the gallbladder or bile duct in the area before the blockage and sew it to the small intestine to create a new pathway around the blocked area.
- Endoscopic stent placement: If the tumor is blocking the bile duct, surgery may be done to put in a stent (a thin tube) to drain bile that has built up in the area.
- The doctor may place the stent through a catheter that drains the bile into a bag on the outside of the body or the stent may go around the blocked area and drain the bile into the small intestine.
- Gastric bypass: If the tumor is blocking the flow of food from the stomach, the stomach may be sewn directly to the small intestine so the patient can continue to eat normally
Radiation therapy
Targeted therapy
Chemotherapy
Chemoradiation therapy
Treatment for Types of Pancreatic Cancers
Also see Treatments
Treatment of resectable or borderline resectable pancreatic cancer may include the following:
- Chemotherapy with or without radiation therapy followed by surgery.
- Surgery.
- Surgery followed by chemotherapy.
- Surgery followed by chemoradiation.
- A clinical trial of chemotherapy and/or radiation therapy before surgery.
- A clinical trial of different ways of giving radiation therapy.
- Surgery to remove the tumor may include Whipple procedure, total pancreatectomy, or distal pancreatectomy.
- Palliative therapy can be started at any stage of disease. pancreatic cancer.
Treatment of pancreatic cancer that is locally advanced may include the following:
- Chemotherapy with or without targeted therapy.
- Chemotherapy and chemoradiation.
- Surgery (Whipple procedure, total pancreatectomy, or distal pancreatectomy).
- Palliative surgery or stent placement to bypass blocked areas in ducts or the small intestine.
- Some patients may also receive chemotherapy and chemoradiation to shrink the tumor to allow for surgery.
- A clinical trial of new anticancer therapies together with chemotherapy or chemoradiation.
- A clinical trial of radiation therapy given during surgery or internal radiation therapy.
- Palliative therapy can be started at any stage of disease.
Treatment of pancreatic cancer that has metastasized or recurred may include the following:
- Chemotherapy with or without targeted therapy.
- Clinical trials of new anticancer agents with or without chemotherapy.
- Palliative therapy can be started at any stage of disease.
Palliative therapy can improve the patient’s quality of life by controlling the symptoms and complications of pancreatic cancer.
Palliative therapy for pancreatic cancer includes the following:
- Palliative surgery or stent placement to bypass blocked areas in ducts or the small intestine.
- Palliative radiation therapy to help relieve pain by shrinking the tumor.
- An injection of medicine to help relieve pain by blocking nerves in the abdomen.
- Other palliative medical care alone.
Possible Side Effects and Risk Factors
Possible Side Effects
- Patients with pancreatic cancer have special nutritional needs.
- Surgery to remove the pancreas may affect its ability to make pancreatic enzymes that help to digest food. As a result, patients may have problems digesting food and absorbing nutrients into the body.
- To prevent malnutrition, the doctor may prescribe medicines that replace these enzymes.
- Pain can occur when the tumor presses on nerves or other organs near the pancreas.
- When pain medicine is not enough, there are treatments that act on nerves in the abdomen to relieve the pain.
- The doctor may inject medicine into the area around affected nerves or may cut the nerves to block the feeling of pain.
- Radiation therapy with or without chemotherapy can also help relieve pain by shrinking the tumor.
- When pain medicine is not enough, there are treatments that act on nerves in the abdomen to relieve the pain.
Risk Factors
Risk factors for pancreatic cancer include the following:
- Smoking.
- Being very overweight.
- Having a personal history of diabetes or chronic pancreatitis.
- Having a family history of pancreatic cancer or pancreatitis.
- Having certain hereditary conditions, such as:
- Multiple endocrine neoplasia type 1 (MEN1) syndrome.
- Hereditary nonpolyposis colon cancer (HNPCC; Lynch syndrome).
- von Hippel-Lindau syndrome.
- Peutz-Jeghers syndrome.
- Hereditary breast and ovarian cancer syndrome.
- Familial atypical multiple mole melanoma (FAMMM) syndrome.
- Ataxia-telangiectasia.
Recovery After Surgery
Information from CETI
Please follow MD/surgeon protocol, as every situation is unique.
Whipple Procedure
Hospital Stay
Full Recovery
Restrictions
Exercise
Total Pancreatectomy
Hospital Stay
3-5 days
Open: 10 days
Full Recovery
Restrictions
Exercise
Exercise Recommendations
Information from the University Hospitals of Leicester
Exercise advice for people after liver and pancreas surgery PDF
Please follow MD/surgeon protocol, as every situation is unique.
Glute squeezes and ankle pumps
- Walking
- Trunk rotation / knee rolling – this will also help release trapped gas
- Pelvic tilt
- Lying down
- Ankle pumps
- SAQ
- Pelvic tilt > bridging
- Sitting:
- Arms:
– Shoulder flexion.
– Arm punches (alternating hands reaching up towards the ceiling.
– Bicep curls with hand weights or soup cans as tolerated - Legs:
- SLAQ
- Arms:
- Standing:
- Marching in place holding onto chair or stable surface
- Six to eight weeks after your operation you can start to do low-impact exercise such as jogging and cycling (on the flat).
- Swimming is another good form of exercise, but please note that your wound must be healed before swimming.
- Start these activities gradually.
- Common sense will guide you as to how much exercise your body can take.
Special Considerations for People with Diabetes
Information from the CDC – Diabetes – Get Active
Please follow MD/surgeon protocol, as every situation is unique.
One of the “side effects” of pancreatic cancer/surgery is diabetes. It is important to understand the correlation between blood sugar and exercise.
Before starting any physical activity, check with your health care provider to talk about the best physical activities for you. Be sure to discuss which activities you like, how to prepare, and what you should avoid.
- Drink plenty of fluids while being physically active to prevent dehydration (harmful loss of water in the body).
- Make sure to check your blood sugar before being physically active, especially if you take insulin.
- If it’s below 100 mg/dL, you may need to eat a small snack containing 15-30 grams of carbohydrates, such as 2 tablespoons of raisins or ½ cup of fruit juice or regular soda (not diet), or glucose tablets so your blood sugar doesn’t fall too low while being physically active.
- Low blood sugar (hypoglycemia) can be very serious.
- If it’s above 240 mg/dL, your blood sugar may be too high (hyperglycemia) to be active safely.
- Test your urine for ketones – substances made when your body breaks down fat for energy.
- The presence of ketones indicates that your body doesn’t have enough insulin to control your blood sugar.
- If you are physically active when you have high ketone levels, you risk ketoacidosis – a serious diabetes complication that needs immediate treatment.
- When you’re physically active, wear cotton socks and athletic shoes that fit well and are comfortable.
- After your activity, check to see how it has affected your blood glucose level.
- After being physically active, check your feet for sores, blisters, irritation, cuts, or other injuries.
- Call your health care provider if an injury doesn’t begin to heal after 2 days.
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
|
Information and pictures from National Cancer Institute unless otherwise specified |