Breast Cancer - Pathology, Staging & Prognosis
Your Body is Your Temple
Research, Resources & Education
Table of Contents
Breast cancer is a complex medical condition that requires a thorough assessment of its severity and progression. To determine the extent of cancer, doctors use a combination of tests and methods, one of which is pathology. Pathology is a specialized medical test that allows doctors to evaluate tissue samples under a microscope, which provides detailed information on the tumor's grade and stage, leading to accurate cancer diagnosis.
Once the grade and stage of breast cancer are determined, doctors can create a treatment plan tailored to each patient's unique needs. The prognosis of breast cancer is an essential part of the treatment plan.
Information and pictures from National Cancer Institute unless otherwise specified
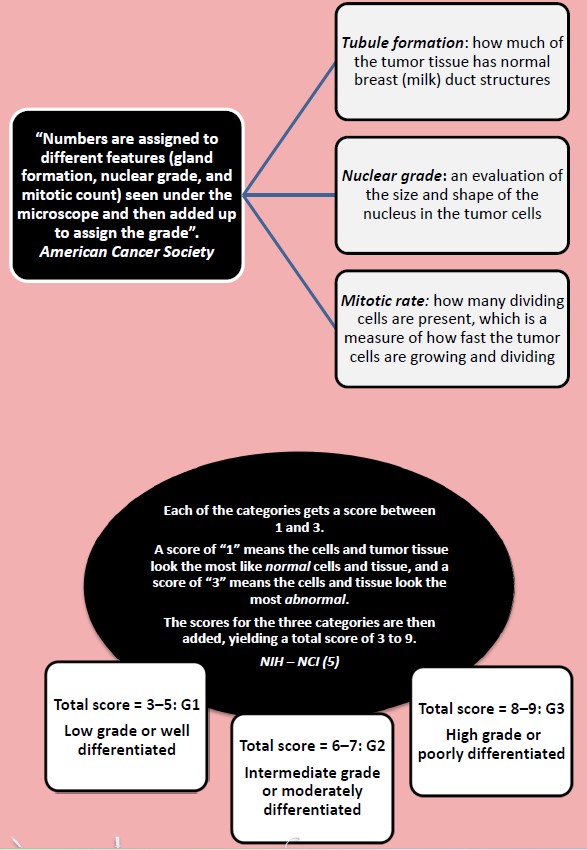
Tumor Grade/ Differentiating Cells
Nottingham Grading System
Staging Systems Videos
YouTube Videos that help explain Staging Systems.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Staging Systems
Staging Systems
Staging
Stage refers to the extent of your cancer, such as how large the tumor is, and if it has spread.
- A cancer is always referred to by the stage it was given at diagnosis, even if it gets worse or spreads.
- New information about how a cancer has changed over time gets added on to the original stage. So, the stage doesn’t change, even though the cancer might.
Systems that Describe Stage
- There are many staging systems. Some, such as the TNM staging system, are used for many types of cancer.
- Others are specific to a particular type of cancer.
- Most staging systems include information about:
- Where the tumor is located in the body
- The cell type (such as, adenocarcinoma or squamous cell carcinoma) • The size of the tumor
- Whether the cancer has spread to nearby lymph nodes
- Whether the cancer has spread to a different part of the body
- Tumor grade, which refers to how abnormal the cancer cells look and how likely the tumor is to grow and spread
TNM Staging System
The TNM system is the most widely used cancer staging system.
- T (Tumor) refers to the size and extent of the main tumor.
- The main tumor is usually called the primary tumor.
- N (Nodes) refers to the number of nearby lymph nodes that have cancer.
- M (Metastasis) refers to whether the cancer has metastasized.
- This means that the cancer has spread from the primary tumor to other parts of the body.
When your cancer is described by the TNM system, there will be numbers after each letter that give more details about the cancer—for example, T1N0MX or T3N1M0. The following explains what the letters and numbers mean:
Primary tumor (T)
- TX: Main tumor cannot be measured.
- T0: Main tumor cannot be found.
- T1, T2, T3, T4: Refers to the size and/or extent of the main tumor.
- The higher the number after the T, the larger the tumor or the more it has grown into nearby tissues.
- T’s may be further divided to provide more detail, such as T3a and T3b.
Regional lymph nodes (N)
- NX: Cancer in nearby lymph nodes cannot be measured.
- N0: There is no cancer in nearby lymph nodes.
- N1, N2, N3: Refers to the number and location of lymph nodes that contain cancer.
- The higher the number after the N, the more lymph nodes that contain cancer.
Distant metastasis (M)
- MX: Metastasis cannot be measured.
- M0: Cancer has not spread to other parts of the body.
- M1: Cancer has spread to other parts of the body.
Stage 0-IV
The TNM system helps describe cancer in great detail. But, for many cancers, the TNM combinations are grouped into five less-detailed stages. When talking about your cancer, your doctor or nurse may describe it as one of these stages:
- Stage 0 or in situ- Abnormal cells are present but have not spread to nearby tissue.
- Also called carcinoma in situ, or CIS.
- CIS is not cancer, but it may become cancer.
- Stage I, Stage II, and Stage III – Cancer is present. The higher the number, the larger the cancer tumor and the more it has spread into nearby tissues.
- Stage IV – The cancer has spread to distant parts of the body.
Localized, Regional, Distant, Unknown
Another staging system that is used for all types of cancer groups the cancer into one of five main categories. This staging system is more often used by cancer registries than by doctors. But, you may still hear your doctor or nurse describe your cancer in one of the following ways:
- Localized—Cancer is limited to the place where it started, with no sign that it has spread.
- Regional—Cancer has spread to nearby lymph nodes, tissues, or organs.
- Distant—Cancer has spread to distant parts of the body.
- Unknown—There is not enough information to figure out the stage.
Prognostic Marker Videos
YouTube Videos that help explain different Prognosis Markers.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Prognosis Markers
Prognostic Markers
Margins or Ink
When an entire tumor is removed, the outside edges (or margins) of the specimen are coated with ink, sometimes even with different colors of ink on different sides of the specimen.
- The pathologist looks at slides of the tumor under the microscope to see how close the cancer cells get to the ink (the edges or margins of the specimen). (American Cancer Society: Understanding Your Pathology Report) •
The margin is described as negative or clean when the pathologist finds no cancer cells at the edge of the tissue, suggesting that all of the cancer has been removed.
- The margin is described as positive or involved when the pathologist finds cancer cells at the edge of the tissue, suggesting that all of the cancer has not been removed. (NCI)
HER2/neu Gene (also IHC and FISH test)
Some breast cancers have too much of a growth-promoting protein called HER2/neu (HER2). The HER2/neu gene instructs the cells to make this protein.
- Tumors with increased levels of HER2/neu are referred to as HER2-positive.
- The cells in HER2-positive breast cancers have too many copies of the HER2/neu gene, resulting in greater than normal amounts of the HER2 protein.
- These cancers tend to grow and spread more quickly than other breast cancers.
- Women with HER2-positive cancers are much more likely to benefit from treatment with drugs that target the HER2 protein.
- If your cancer is HER2-positive, your doctor might add certain drugs to your treatment.
- How the results of your tests will affect your treatment is best discussed with your doctor.
Testing of the biopsy or surgery sample:
- Immunohistochemistry (IHC): In this test, special antibodies that will stick to the HER2 protein are applied to the sample, which cause cells to change color if many copies are present.
- This color change can be seen under a microscope.
- The test results are reported as 0, 1+, 2+, or 3+. • 0 or 1+:
- HER2- (negative). Women with HER2- negative tumors are not treated with drugs that target HER2. •
- 3+ : HER2 + (positive). The person might benefit from treatment with drugs that target HER2.
- 2+: HER2 status of the tumor is not clear and is called “equivocal.” This means that the HER2 status needs to be tested with FISH to clarify the result.
- Fluorescent in situ hybridization (FISH): This test uses fluorescent pieces of DNA that specifically stick to copies of the HER2/neu gene in cells, which can then be counted under a special microscope.
- Chromogenic in situ hybridization (CISH): This test works similarly to FISH, by using small DNA probes to count the number of HER2/neu genes in breast cancer cells.
(American Cancer Society: Understanding Your Pathology Report)
Estrogen Receptor (ER)
Estrogen: A type of hormone made by the body that helps develop and maintain female sex characteristics and the growth of long bones.
- Estrogens can also be made in the laboratory.
- They may be used as a type of birth control and to treat symptoms of menopause, menstrual disorders, osteoporosis, and other conditions.
Estrogen receptor (ER): A protein found inside the cells of the female reproductive tissue, some other types of tissue, and some cancer cells.
- The hormone estrogen will bind to the receptors inside the cells and may cause the cells to grow.
- Also called ER.
Estrogen receptor negative (ER-): Describes cells that do not have a protein to which the hormone estrogen will bind.
- Cancer cells that are estrogen receptor negative do not need estrogen to grow, and usually do not stop growing when treated with hormones that block estrogen from binding.
- Also called ER negative.
Estrogen receptor positive (ER+): Describes cells that have a receptor protein that binds the hormone estrogen.
- Cancer cells that are estrogen receptor positive may need estrogen to grow, and may stop growing or die when treated with substances that block the binding and actions of estrogen.
- Also called ER positive.
Estrogen receptor (ER) test: A lab test to find out if cancer cells have estrogen receptors (proteins to which estrogen will bind).
- If the cells have estrogen receptors, they may need estrogen to grow, and this may affect how the cancer is treated. (NCI)
Results for ER are reported separately and can be reported in different ways:
- Negative, weakly positive, positive
- Percent positive
- Percent positive and whether the staining is weak, moderate, or strong.
Women with hormone receptor-positive cancers tend to have a better prognosis and are much more likely to respond to hormone therapy than women with cancers without these receptors.
(American Cancer Society: Understanding Your Pathology Report)
Progesterone Receptor (PR)
Progesterone: A type of hormone made by the body that plays a role in the menstrual cycle and pregnancy.
- Progesterone can also be made in the laboratory.
- It may be used as a type of birth control and to treat menstrual disorders, infertility, symptoms of menopause, and other conditions.
Progesterone receptor (PR): A protein found inside the cells of the female reproductive tissue, some other types of tissue, and some cancer cells.
- The hormone progesterone will bind to the receptors inside the cells and may cause the cells to grow.
- Also called PR. •
Progesterone receptor negative (PR-): Describes cells that do not have a protein to which the hormone progesterone will bind.
- Cancer cells that are progesterone receptor negative do not need progesterone to grow, and usually do not stop growing when treated with hormones that block progesterone from binding.
- Also called PR negative.
Progesterone receptor positive (PR+): Describes cells that have a protein to which the hormone progesterone will bind.
- Cancer cells that are progesterone receptor positive need progesterone to grow and will usually stop growing when treated with hormones that block progesterone from binding.
- Also called PR positive.
Progesterone receptor (PR) test: A lab test to find out if cancer cells have progesterone receptors (proteins to which the hormone progesterone will bind).
- If the cells have progesterone receptors, they may need progesterone to grow, and this can affect how the cancer is treated. (NCI)
Results for PR are reported separately and can be reported in different ways:
- Negative, weakly positive, positive
- Percent positive
- Percent positive and whether the staining is weak, moderate, or strong.
Women with hormone receptor-positive cancers tend to have a better prognosis and are much more likely to respond to hormone therapy than women with cancers without these receptors.
(American Cancer Society: Understanding Your Pathology Report)
Ki-67
Ki-67 is a way to measure how fast the cancer cells are growing and dividing.
- High values (over 30%) for Ki-67 mean that many cells are dividing, so the cancer is likely to grow and spread more quickly”. (American Cancer Society: Understanding Your Pathology Report)
- Less than 10% – low • 10-20/25% – borderline,
- More than 20-25% – high
- The higher the percentage, the more aggressive the cancer is. (BreastCancer.org: Rate of Cell Growth)
S-phase Fraction
This number tells you what percentages of cells in the sample are in the process of copying their genetic information, or DNA. This S-phase, short for “synthesis phase,” happens just before a cell divides into two new cells. (BreastCancer.org: Rate of Cell Growth)
- Less than 6% – low
- 6-10% – intermediate
- More than 10% – high.
Lymphovascular Invasion
Lymphovascular invasion (LVI) is defined as the presence of tumor cells within a definite endothelial-lined space (lymphatics or blood vessels) in the breast surrounding invasive carcinoma.
- The presence of LVI is associated with an increased risk of axillary lymph node and distant metastases.
- Although the mechanism of LVI has not been completely elucidated, LVI is considered as a prognostic factor in patients with operable breast cancer with or without metastatic axillary lymph nodes who are undergoing adjuvant treatment. (NCBI – PMC Lymphovascular invasion)
Multigene tests
Tests in which samples of tissue are studied to look at the activity of many genes at the same time.
- These tests may help predict whether cancer will spread to other parts of the body or recur (come back).
- There are many types of multigene tests. The following multigene tests have been studied in clinical trials:
Oncotype DX: This test helps predict whether early-stage breast cancer that is estrogen receptor positive and node negative will spread to other parts of the body.
- If the risk that the cancer will spread is high, chemotherapy may be given to lower the risk.
MammaPrint: A laboratory test in which the activity of 70 different genes is looked at in the breast cancer tissue of women who have early-stage invasive breast cancer that has not spread to lymph nodes or has spread to 3 or fewer lymph nodes.
The activity level of these genes helps predict whether breast cancer will spread to other parts of the body or come back.
If the test shows that the risk that the cancer will spread or come back is high, chemotherapy may be given to lower the risk. (NCI)
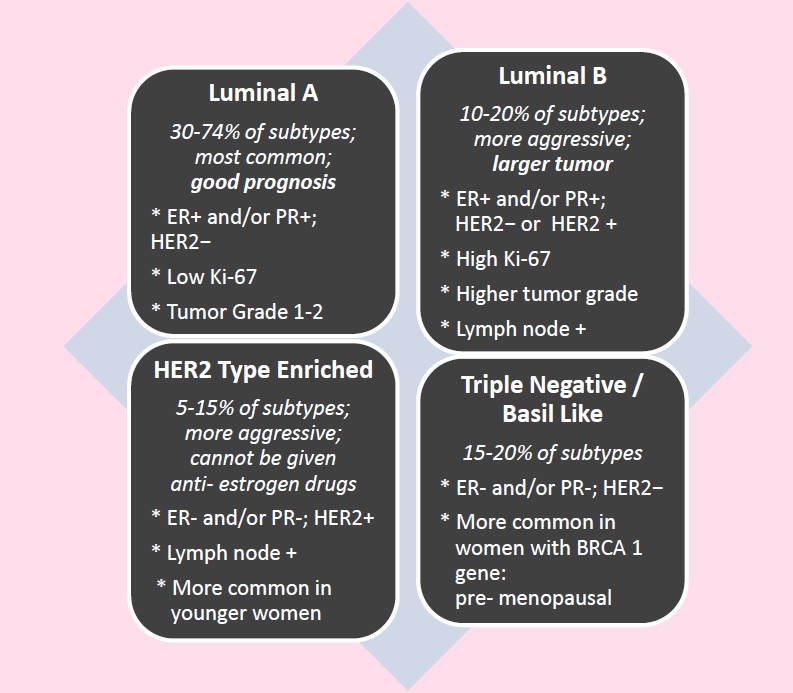
Molecular Subtypes - See diagram below
Four main breast cancer subtypes have been identified according to estrogen receptor (ER), progesterone receptor (PR), and HER2.
- These subtypes include luminal types A and B, basal-like, and HER2-enriched subtype.
Molecular Subtypes - Diagram
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
Information and pictures from National Cancer Institute unless otherwise specified