Breast Cancer
Exercises, Precautions & Contraindications
Your Body is Your Temple
Research, Resources & Education
Table of Contents
If you had surgery for breast reconstruction, there are some exercise precautions you should keep in mind. These precautions are important if you had surgery using the TRAM, DIEP, or LAT flap methods, tissue expanders, or if you have lymphedema, neuropathy, or nerve damage. It's important to follow these precautions to avoid injury and allow your body to heal properly. Speak with your doctor or physical therapist to learn more about what exercises are safe and which ones you should avoid.
Information and pictures from National Cancer Institute unless otherwise specified
Post Mastectomy Exercises after Surgery Videos
YouTube Videos that help explain Exercises after Surgery.
It is extremely important that you follow your MD or physical therapists exercise and post surgerical recommendations, as each surgery may have it’s own protocol or complications.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Post Mastectomy Exercise
TRAM, LAT & DIEP Flap / Tissue Expanders
Information from CETI and BreastCancer.org
Please follow MD/surgeon protocol, as every situation is unique.

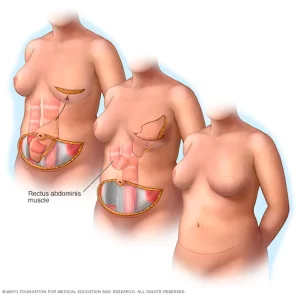
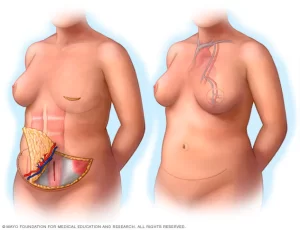
TRAM Flap Reconstruction
TRAM stands for the transverse rectus abdominis muscle, which is located in the lower abdomen, between the waist and the pubic bone.
- A TRAM flap uses a part of this muscle, its blood vessels, and some belly fat to rebuild the breast.
- After TRAM flap surgery, you can start walking the next day, though it will probably hurt because of the incision in your abdomen.
- For the first two days, many physical therapists recommend women do calf exercises and deep breathing exercises to help prevent blood clots.
- You can start arm rehabilitation exercises 3 or 4 days after surgery.
- Once the drains are removed, you can start stretching your chest, shoulders, and arms.
- It’s also a good idea to walk regularly as you recover.
- Don’t do any abdominal (“abs”) exercises until about 6 weeks after surgery or whenever your surgeon says it’s OK to start.
- Start slowly and gently while continuing your stretching exercises and walking or other low-intensity aerobic exercise.
- Those with a unilateral TRAM Flap may need minor assistance in lowering themselves back onto the floor.
- Bi-lateral Tram Flap, will not be able to roll backwards or subsequently roll back to an upright position without assistance
BreastCancer.org and CETI (Pilates)
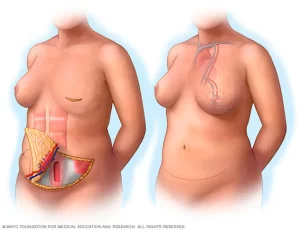
DIEP Flap Reconstruction
DIEP stands for deep inferior epigastric perforator. In a DIEP flap, fat, skin, and blood vessels, but no muscles, are cut from the wall of the lower belly and moved up to your chest to rebuild your breast.
- After DIEP flap surgery, you can start walking the next day, though it will probably hurt because of the incision in your abdomen.
- For the first 2 days, many physical therapists recommend women do calf exercises and deep breathing exercises to help prevent blood clots.
- You can start arm rehabilitation exercises 3 or 4 days after surgery. • Once the drains are removed, you can start stretching your chest, shoulders, and arms.
- It’s also a good idea to walk regularly as you recover.
- Don’t do any abdominal (“abs”) exercises until about 6 weeks after surgery or whenever your surgeon says it’s OK to start.
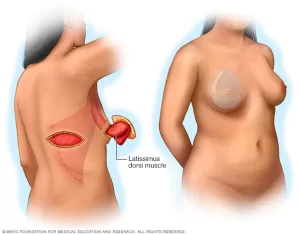
LAT Flap Reconstruction
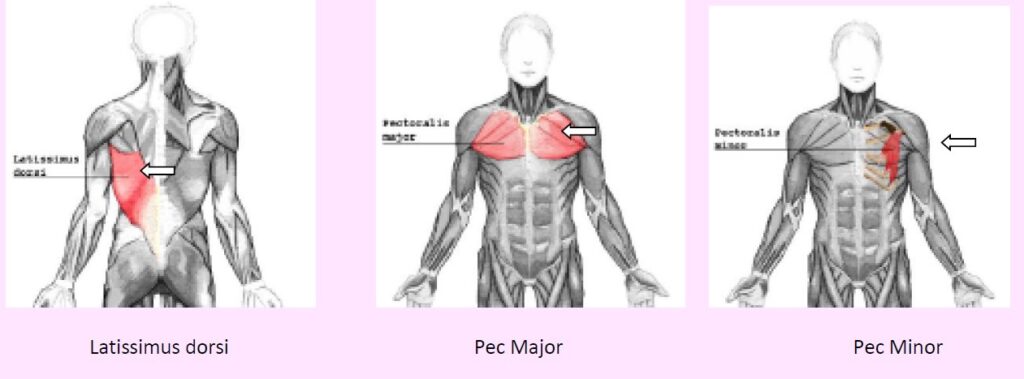
The latissimus dorsi is the muscle below the shoulder and behind the armpit. A latissimus dorsi flap uses an oval section of this muscle, skin, and fat to rebuild the breast.
- Because this type of reconstruction affects the shoulder muscle, you should wait to start any gentle shoulder stretching until about 2 weeks after surgery.
- Wait until about 3 months after surgery to do any resistance/strength exercises.
- If you have any shortness of breath, pain, or tightness in your chest, stop exercising immediately. Tell your doctor what happened and work with him or her to develop a plan of movements that are right for you.
- LAT Flap – may have noticeable weakness and instability in the affected shoulder(s).
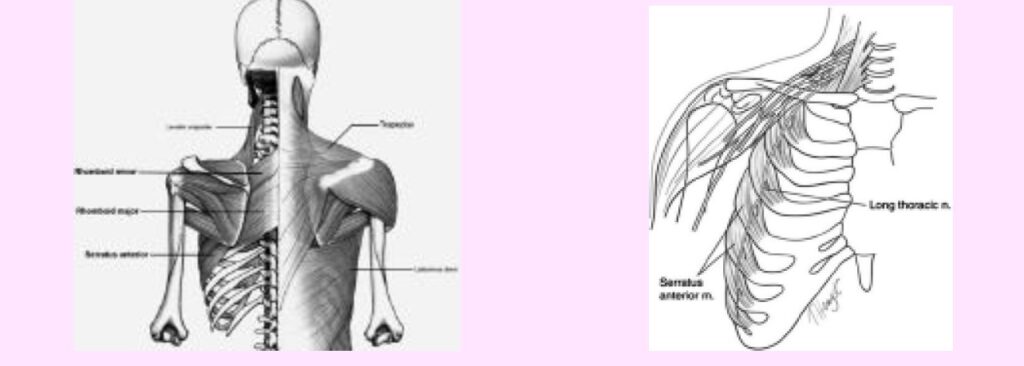
- Retract the shoulders prior to initiating the movement. This will help to contract the rhomboids and other scapular stabilizers.
- Keep in mind that if you had a LAT Flap that one, or both, of the latissimus muscles are now in their chest wall. Because they are still “attached,” they may feel a contraction in their chest when back exercises are performed.
BreastCancer.org and CETI (Pilates)
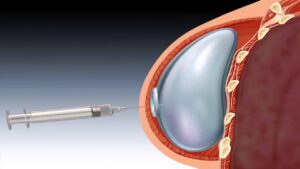
Tissue Expander
If you have a tissue expander in (a temporary inflatable implant that stretches the skin to make room for the final implant), you can usually start gentle shoulder stretching exercises about 2 weeks after surgery once your mastectomy scar has started to heal.
- Many physical therapists recommend doing these stretches right after a warm shower because the muscles and skin are more flexible.
- If you have expanders or breast implants, you will want to begin with limited ROM. It is rare, but possible, that the implants will move out of their “pocket,” and need surgical correction.
- No chest exercises when tissue expanders are in place.
BreastCancer.org and CETI (Pilates)
Lymphedema and Exercise
Both light exercise and aerobic exercise (physical activity that causes the heart and lungs to work harder) help the lymph vessels move lymph out of the affected limb and decrease swelling.
- If you have lymphedema or are at risk, talk with a certified lymphedema therapist before beginning exercise. This includes anyone who has had lymph nodes removed or radiation.
- Patients who have lymphedema or who are at risk for lymphedema should talk with a certified lymphedema therapist before beginning an exercise routine.
- See the Lymphology Association of North America web site for a list of certified lymphedema therapists in the US
- Wear a pressure garment if lymphedema has developed.
- Patients who have lymphedema should wear a well-fitting pressure garment during all exercise that uses the affected limb or body part.
- When it is not known for sure if a woman has lymphedema, upper-body exercise without a garment may be more helpful than no exercise at all.
- Patients who do not have lymphedema do not need to wear a pressure garment during exercise.
- Avoid wrapping a band around your hand when using for resistance. This will put you at risk for increased edema by cutting off the circulation. Hold the band or use a band that has handles.
- Breast cancer survivors should begin with light upper-body exercise and increase it slowly.
- Some studies with breast cancer survivors show that upper-body exercise is safe in women who have lymphedema or who are at risk for lymphedema.
- Weight-lifting that is slowly increased may keep lymphedema from getting worse.
- Exercise should start at a very low level, increase slowly over time, and be overseen by the lymphedema therapist.
- If exercise is stopped for a week or longer, it should be started again at a low level and increased slowly.
- If symptoms (such as swelling or heaviness in the limb) change or increase for a week or longer, talk with the lymphedema therapist.
- It is likely that exercising at a low level and slowly increasing it again over time is better for the affected limb than stopping the exercise completely.
- More studies are needed to find out if weight-lifting is safe for cancer survivors with lymphedema in the legs.
Axillary Lymph Node Dissection & Scar Tissue
If you have undergone an axillary node dissection, or radiation/dissection to the nodes in the neck, you may struggle with scar tissue/adhesions in that area.
- Gently ease into the stretch and only go as far as you can, with mild discomfort, but NO pain
- Start with a few repetitions and gradually increase as tolerated (no swelling).
Also see Lymphedema Section
Nerve Damage
Peripheral Neuropathy
- Some cancer treatments cause peripheral neuropathy, a result of damage to the peripheral nerves.
- These nerves carry information from the brain to other parts of the body.
- Feet or lower extremity – caution with standing on uneven surface, such as a Bosu ball or balance pads due to decreased sensation in feet. Increased risk of falling.
- Hands – caution with holding dumbbells or grasping resistance bands.
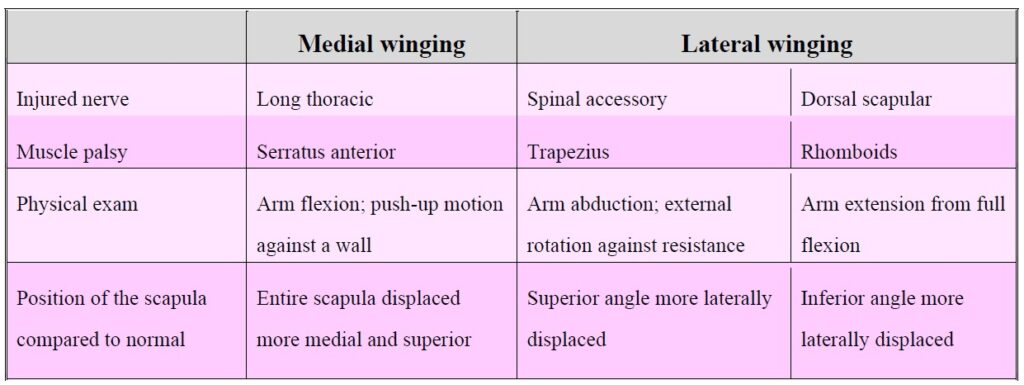
Nerves that may be Damaged during Surgery by Pink Ribbon Program©
Several structures, including vessels and muscles with their nerve supply, are related to the breast and should be preserved during mastectomy or axillary node dissection.
- The lateral pectoral nerve passes medially around the medial pectoralis minor, and the medial pectoral nerve passes laterally around the pectoralis minor.
- These nerves can be severed during surgery.
- This results in numbness, motor atrophy, decreased sweat production in armpit and arm.
- The medial pectoral nerve innervates pectoralis minor and the lateral portion of the pectoralis major muscles.
- Preservation of this nerve is particularly important to prevent atrophy of the pectoral muscles if submuscular implant reconstruction is planned.
- The thoracodorsal nerve is identifiable medial to the thoracodorsal vein.
- Injury may result in a weakening of the latissimus.
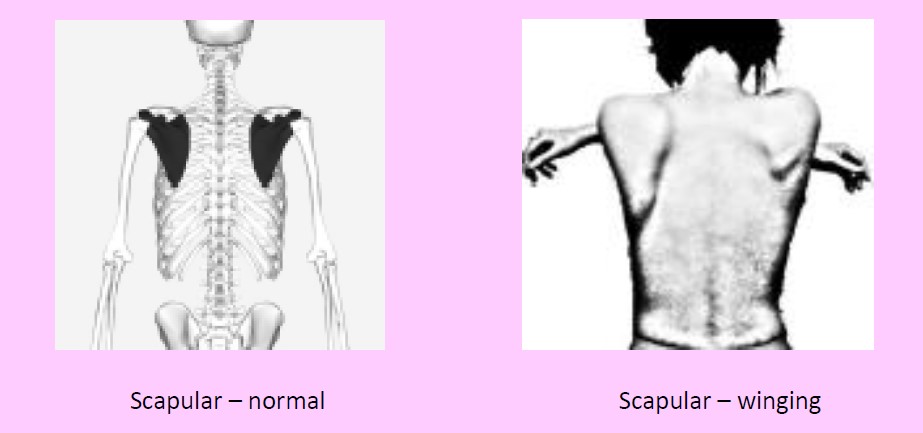
- The long thoracic nerve of Bell is located more medially in the axilla.
- It runs just beneath the fascia of the serratus anterior, medial to the thoracodorsal complex.
- Injury to this nerve will result in weakness in the serratus and cause winging of the scapula.
Neurogenic Causes of Scapular Winging & the Physical Exam / Diagrams
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
|
Information and pictures from National Cancer Institute unless otherwise specified |