Prostate Cancer
Your Body is Your Temple
Research, Resources & Education
Table of Contents
Prostate cancer is a serious threat to men's health. It develops in the prostate gland, causing discomfort, pain, and complications. With certain risk factors, it can lead to a malignant tumor that spreads quickly. Early detection and treatment can increase chances of recovery and prevention of severe complications. Men should be vigilant about their health and have regular medical check-ups to monitor their prostate gland.
Information and pictures from National Cancer Institute unless otherwise specified
Prostate Anatomy & Normal vs. Enlarged
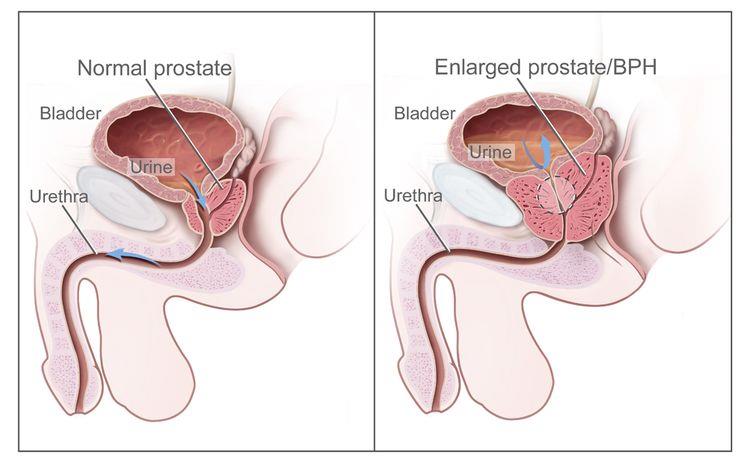
(See Pic)
The prostate is a gland in the male reproductive system.
- It lies just below the bladder (the organ that collects and empties urine) and in front of the rectum (the lower part of the intestine).
- It is about the size of a walnut and surrounds part of the urethra (the tube that empties urine from the bladder).
- The prostate gland makes fluid that is part of the semen.
- Normal prostate and benign prostatic hyperplasia (BPH).
- A normal prostate does not block the flow of urine from the bladder.
- An enlarged prostate presses on the bladder and urethra and blocks the flow of urine.
Prostate Cancer Videos
YouTube Videos that help explain Prostate Cancer.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Prostate Cancer
Treatments
Also see Treatments
Patients in good health whose tumor is in the prostate gland only may be treated with surgery to remove the tumor. The following types of surgery are used:
A surgical procedure to remove the prostate, surrounding tissue, and seminal vesicles.
There are two types of radical prostatectomy:
- Retropubic prostatectomy: A surgical procedure to remove the prostate through an incision (cut) in the abdominal wall.
- Removal of nearby lymph nodes may be done at the same time.
- Perineal prostatectomy: A surgical procedure to remove the prostate through an incision (cut) made in the perineum (area between the scrotum and anus).
- Nearby lymph nodes may also be removed through a separate incision in the abdomen
A surgical procedure to remove the lymph nodes in the pelvis.
- A pathologist views the tissue under a microscope to look for cancer cells.
- If the lymph nodes contain cancer, the doctor will not remove the prostate and may recommend other treatment.
A surgical procedure to remove tissue from the prostate using a resectoscope (a thin, lighted tube with a cutting tool) inserted through the urethra.
- This procedure is done to treat benign prostatic hypertrophy and it is sometimes done to relieve symptoms caused by a tumor before other cancer treatment is given.
- TURP may also be done in men whose tumor is in the prostate only and who cannot have a radical prostatectomy.
Radiopharmaceutical therapy uses a radioactive substance to treat cancer including:
- Alpha emitter radiation therapy, which uses a radioactive substance to treat prostate cancer that has spread to the bone.
- A radioactive substance called radium-223 is injected into a vein and travels through the bloodstream.
- The radium-223 collects in areas of bone with cancer and kills the cancer cells.
Cryosurgery is a treatment that uses an instrument to freeze and destroy prostate cancer cells.
- Ultrasound is used to find the area that will be treated.
- Cryosurgery can cause impotence and leakage of urine from the bladder or stool from the rectum.
High-intensity–focused ultrasound therapy is a treatment that uses ultrasound (high-energy sound waves) to destroy cancer cells.
- To treat prostate cancer, an endorectal probe is used to make the sound waves.
Proton beam radiation therapy is a type of high-energy, external radiation therapy that targets tumors with streams of protons (small, positively charged particles).
- This type of radiation therapy is being studied in the treatment of prostate cancer.
Hormone therapy Hormone therapy is a cancer treatment that removes hormones or blocks their action and stops cancer cells from growing.
- Hormones are substances made by glands in the body and circulated in the bloodstream.
- In prostate cancer, male sex hormones can cause prostate cancer to grow.
- Drugs, surgery, or other hormones are used to reduce the amount of male hormones or block them from working. This is called androgen deprivation therapy (ADT).
Hormone therapy for prostate cancer may include the following:
- Abiraterone acetate can prevent prostate cancer cells from making androgens.
- It is used in men with advanced prostate cancer that has not gotten better with other hormone therapy.
- It is also used in men with high-risk prostate cancer that has improved with treatments that lower hormone levels.
- Orchiectomy is a surgical procedure to remove one or both testicles, the main source of male hormones, such as testosterone, to decrease the amount of hormone being made.
- Estrogens (hormones that promote female sex characteristics) can prevent the testicles from making testosterone.
- However, estrogens are seldom used today in the treatment of prostate cancer because of the risk of serious side effects..
- Luteinizing hormone-releasing hormone agonists can stop the testicles from making testosterone.
- Examples are leuprolide, goserelin, and buserelin.
- Antiandrogens can block the action of androgens (hormones that promote male sex characteristics), such as testosterone.
- Examples are flutamide, bicalutamide, enzalutamide, apalutamide, nilutamide, and darolutamide.
- Drugs that can prevent the adrenal glands from making androgens include ketoconazole, aminoglutethimide, hydrocortisone, and progesterone.
Radiation therapy
Targeted therapy
Chemotherapy
Watchful waiting or active surveillance
Biologic therapy
Bisphosphonate therapy
Possible Side Effects & Risk Factors
Information also from the Mayo Clinic
Possible Side Effects
SURGERY:
- Transurethral resection of the prostate (TURP)
- Recurring urinary tract infections
- Kidney or bladder damage
- Inability to control urination or an inability to urinate at all
- Bladder stones
- Blood in your urine (Mayo)
- Radical prostatectomy
- Impotence
- Heart attack / stroke
- Bladder spasms
- Blood clot in the legs
- Leakage of urine from the bladder or stool from the rectum.
- Shortening of the penis (1 to 2 centimeters). The exact reason for this is not known.
- Inguinal hernia (bulging of fat or part of the small intestine through weak muscles into the groin).
- Inguinal hernia may occur more often in men treated with radical prostatectomy than in men who have some other types of prostate surgery, radiation therapy, or prostate biopsy alone.
- It is most likely to occur within the first 2 years after radical prostatectomy.
- Pelvic lymphadenectomy: If lymph nodes are removed, there may be additional side effects:
- Lymphedema •
- Seroma
- Infection
- Nerve damage
Bone Pain:
- Prostate cancer that has spread to the bone and certain types of hormone therapy can weaken bones and lead to bone pain.
- Treatments for bone pain include the following:
- Pain medicine.
- External radiation therapy.
- Strontium-89 (a radioisotope).
- Targeted therapy with a monoclonal antibody, such as denosumab.
- Bisphosphonate therapy.
- Corticosteroids.
Radiation therapy:
- Increased risk of bladder and/or gastrointestinal cancer.
- Can also cause impotence and urinary problems that may get worse with age.
Hormone therapy:
- Hot flashes, impaired sexual function, loss of desire for sex, and weakened bones
Cryosurgery:
- Can cause impotence and leakage of urine from the bladder or stool from the rectum
Risk Factors
Age
- Age is an important risk factor for prostate cancer.
- Prostate cancer is rarely seen in men younger than 40 years; the incidence rises rapidly with each decade thereafter.
- For example, the probability of being diagnosed with prostate cancer is 1 in 456 for men 49 years or younger, 1 in 54 for men aged 50 through 59 years, 1 in 19 for men aged 60 through 69 years, and 1 in 11 for men aged 70 years and older, with an overall lifetime risk of developing prostate cancer of 1 in 8.
Ancestry
- The risk of developing and dying from prostate cancer is higher among Black men, is of intermediate levels among White men, and is lowest among native Japanese.
- Conflicting data have been published regarding the etiology of these outcomes, but some evidence is available that access to health care may play a role in disease outcomes.
- According to the Surveillance, Epidemiology, and End Results (SEER) Program, incidence of prostate cancer in African American men exceeds those of White men at all ages.
Family History
- Approximately 15% of men with a diagnosis of prostate cancer will be found to have a first-degree relative (e.g., brother, father) with prostate cancer, compared with approximately 8% of the U.S. population.
- Approximately 9% of all prostate cancers may result from heritable susceptibility genes.
Other Risks
- Hormones
- Dietary Fat
- Dairy and Calcium Intake
- Multivitamin Use
- Folate
- Cadmium Exposure
- Dioxin Exposure
- Prostatitis
Recovery After Surgery
Information from CETI
Some information also from the Mayo Clinic
Transurethral resection of the prostate (TURP)
Please follow MD/surgeon protocol, as every situation is unique.
Radical Prostatectomy
Hospital Stay
Full Recovery
Restrictions
Exercise
(See Kegel)
Other
Transurethral Resection of the Prostate (TURP)
Hospital Stay
Full Recovery
Restrictions
Exercise
(See Kegel)
Other
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
|
Information and pictures from National Cancer Institute unless otherwise specified |