Sentinal / Axillary Lymph Nodes & Cancer
Your Body is Your Temple
Research, Resources & Education
Table of Contents
The sentinel lymph node identifies where cancer cells accumulate and plays a crucial role in determining treatment options. It's typically the first lymph node near the primary tumor. Knowing its function and significance is vital for effective cancer treatment.
Information and pictures from National Cancer Institute unless otherwise specified
Sentinel Lymph Nodes
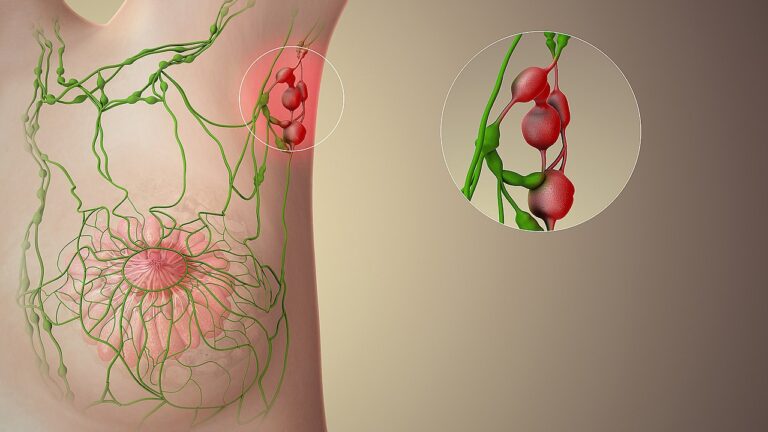
- A sentinel lymph node is defined as the first lymph node to which cancer cells are most likely to spread from a primary tumor.
- Sometimes, there can be more than one sentinel lymph node.
- Lymph nodes are small round organs that are part of the body’s lymphatic system.
- The lymphatic system is a part of the immune system.
- It consists of a network of vessels and organs that contains lymph, a clear fluid that carries infection-fighting white blood cells as well as fluid and waste products from the body’s cells and tissues.
- In a person with cancer, lymph can also carry cancer cells that have broken off from the main tumor.
Videos of Sentinel & Axillary Lymph Nodes, Biopsy & Surgery
YouTube Videos that help explain Sentinel & Axillary Lymph Nodes, Biopsy & Surgery.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Sentinel & Axillary Lymph Nodes
Sentinel Lymph Nodes Biopsy (SLNB) & Surgery
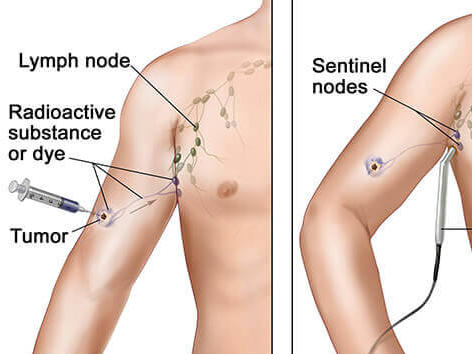
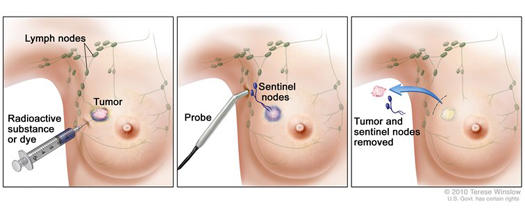
- A sentinel lymph node biopsy (SLNB) is a procedure in which the sentinel lymph node is identified, removed, and examined to determine whether cancer cells are present.
- It is used in people who have already been diagnosed with cancer.
- A negative SLNB result suggests that cancer has not yet spread to nearby lymph nodes or other organs.
- A positive SLNB result indicates that cancer is present in the sentinel lymph node and that it may have spread to other nearby lymph nodes (called regional lymph nodes) and, possibly, other organs.
- This information can help a doctor determine the stage of the cancer (extent of the disease within the body) and develop an appropriate treatment plan.
- First, the surgeon injects a dye, a radioactive tracer, or both into the breast near the tumor. This helps the surgeon see which lymph nodes the lymph from that area of the breast flows to first.
- Then, he or she removes the node or nodes that contain the dye or radioactive tracer to see if they have cancer.
- If they do not contain cancer, it is not likely that the other nodes under the arm have cancer. This means that the surgeon usually doesn’t have to remove any other lymph nodes.
- If cancer is found, the surgeon may remove additional lymph nodes, either during the same biopsy procedure or during a follow-up surgical procedure. SLNB may be done on an outpatient basis or may require a short stay in the hospital.
- Fewer lymph nodes are removed with sentinel lymph node biopsy than with standard lymph node surgery.
- Having fewer lymph nodes removed helps lower the chances that you will develop lymphedema and other problems caused by damage to lymph vessels and lymph nodes.
SLN & Breast Cancer
Breast cancer cells are most likely to spread first to lymph nodes located in the axilla, or armpit area, next to the affected breast. However, in breast cancers close to the center of the chest (near the breastbone), cancer cells may spread first to lymph nodes inside the chest (under the breastbone, called internal mammary nodes) before they can be detected in the axilla.
- The number of lymph nodes in the axilla varies from person to person; the usual range is between 20 and 40.
- Historically, all of these axillary lymph nodes were removed (in an operation called axillary lymph node dissection, or ALND) in women diagnosed with breast cancer.
- This was done for two reasons:
- Help stage the breast cancer
- Help prevent a regional recurrence of the disease. (Regional recurrence of breast cancer occurs when breast cancer cells that have migrated to nearby lymph nodes give rise to a new tumor.)
- This was done for two reasons:
- However, because removing multiple lymph nodes at the same time increases the risk of harmful side effects, clinical trials were launched to investigate whether just the sentinel lymph nodes could be removed.
- Two NCI-sponsored randomized phase 3 clinical trials have shown that SLNB without ALND is sufficient for staging breast cancer and for preventing regional recurrence in women who have no clinical signs of axillary lymph node metastasis, such as a lump or swelling in the armpit that may cause discomfort, and who are treated with surgery, adjuvant systemic therapy, and radiation therapy.
Benefits and Risks of SLNB
- SNLB helps doctors stage cancers and estimate the risk that tumor cells have developed the ability to spread to other parts of the body.
- If the sentinel node is negative for cancer, a patient may be able to avoid more extensive lymph node surgery, reducing the potential complications associated with having many lymph nodes removed.
All surgery to remove lymph nodes, including SLNB, can have harmful side effects, although removal of fewer lymph nodes is usually associated with fewer side effects, particularly serious ones such as lymphedema.
The potential side effects include:
- Lymphedema (see lymphedema). During lymph node surgery, lymph vessels leading to and from the sentinel node or group of nodes are cut. This disrupts the normal flow of lymph through the affected area, which may lead to an abnormal buildup of lymph fluid that can cause swelling.
- The risk of lymphedema increases with the number of lymph nodes removed. There is less risk with the removal of only the sentinel lymph node.
- In the case of extensive lymph node removal in an armpit or groin, the swelling may affect an entire arm or leg.
- In addition, there is an increased risk of infection in the affected area or limb.
- Very rarely, chronic lymphedema due to extensive lymph node removal may cause a cancer of the lymphatic vessels called lymphangiosarcoma.
- Seroma – a mass/ lump caused by the buildup of lymph fluid at the site of the surgery.
- Numbness, tingling, swelling, bruising, or pain at the site of the surgery, and an increased risk of infection
- Difficulty moving the affected body part
- Skin or allergic reactions to the blue dye used in SNLB
- A false-negative biopsy result—that is, cancer cells are not seen in the sentinel lymph node even though they have already spread to regional lymph nodes or other parts of the body. A false-negative biopsy result gives the patient and the doctor a false sense of security about the extent of cancer in the patient’s body.
Axillary Lymph Nodes, Levels, Dissection and Risk
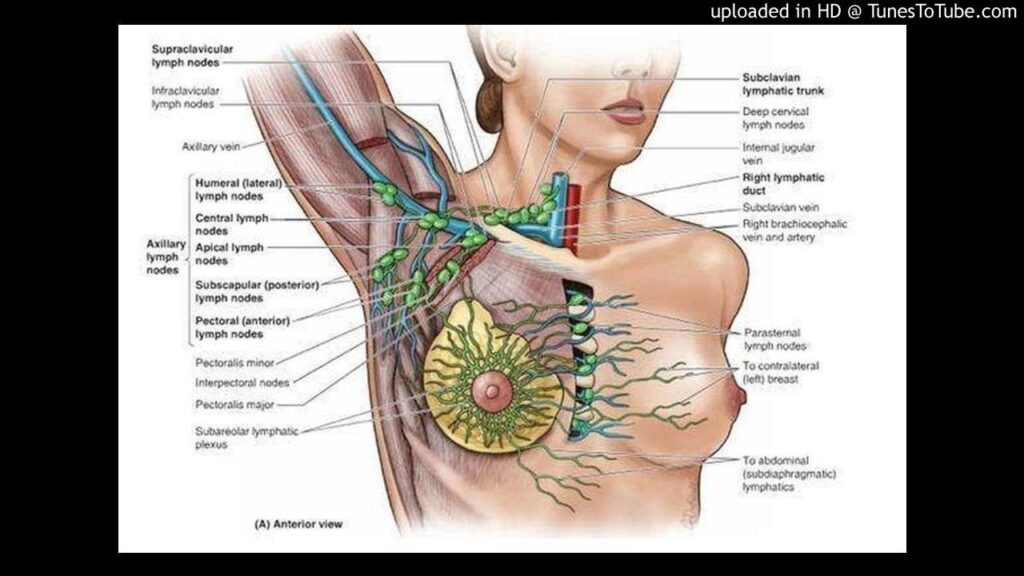
The axillary lymph nodes or armpit lymph nodes are lymph nodes in the human armpit.
- Between 20 and 49 in number.
- They drain lymph vessels from the lateral quadrants of the breast, the superficial lymph vessels from thin walls of the chest and the abdomen above the level of the navel, and the vessels from the upper limb.
- They are divided in several groups according to their location in the armpit. These lymph nodes are clinically significant in breast cancer, and metastases from the breast to the axillary lymph nodes are considered in the staging of the disease.
- About 75% of lymph from the breasts drains into the axillary lymph nodes, making them important in the diagnosis and staging of breast cancer.
- A doctor will usually refer a patient to a surgeon to have an axillary lymph node dissection to see if the cancer cells have been trapped in the nodes.
- For clinical stages I and II breast cancer, axillary lymph node dissection should only be performed after first attempting sentinel node biopsy.
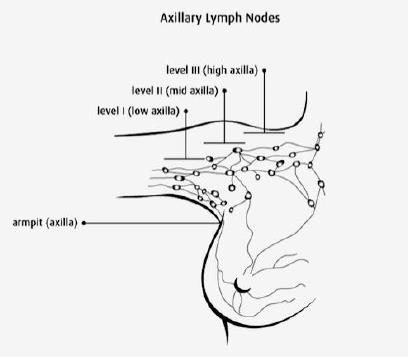
The three levels of an axillary lymph node dissection, from least aggressive to most aggressive, are:
- Level I– The surgical removal of all tissue below the lower edge of the pectoralis minor muscle.
- Level II– The surgical removal of the tissue lying underneath the pectoralis minor muscle.
- Level III – The most aggressive dissection and is the surgical removal of tissue lying above the pectoralis minor muscle.
A traditional axillary lymph node dissection usually includes removal of the nodes in levels I and II from the “fat pad” under the arm.
UPMC- Axillary Lymph Node Dissection
Surgical Margin for Fat Pad:
- Axillary vein – Superior
- Thoracodorsal bundle – Lateral
- Long thoracic nerve – Medial
Anywhere from about 10 to 40 (though usually less than 20) lymph nodes are removed from the area under the arm (axilla) and checked for cancer spread.
- ALND is usually done at the same time as a mastectomy or breast-conserving surgery (BCS), but it can be done in a second operation. ALND may be needed:
- If a previous SLNB has shown 3 or more of the underarm lymph nodes have cancer cells
- If swollen underarm or collarbone lymph nodes can be felt before surgery or seen on imaging tests and a FNA or core needle biopsy shows cancer.
- If the cancer has grown large enough to extend outside the lymph node(s)
- If the SLNB is positive for cancer cells after chemotherapy was given to shrink the tumor before surgery. American Cancer Society
- Compared with axillary sampling alone, partial or total mastectomy followed by full axillary lymph node dissection significantly increases a patient’s chance of developing arm edema.
- In one series of 100 women who underwent partial or total mastectomy and then full axillary lymph node dissection or axillary sampling, arm edema developed in more patients who underwent axillary lymph node dissection compared with sampling alone (30% vs. none). In
addition, the extent of axillary lymph node dissection increases the risk for developing arm edema.
Nerves that may be Damaged during Surgery
Information From Pink Ribbon Program©
Several structures, including vessels and muscles with their nerve supply, are related to the breast and should be preserved during mastectomy or axillary node dissection.
- The lateral pectoral nerve passes medially around the medial pectoralis minor, and the medial pectoral nerve passes laterally around the pectoralis minor These nerves can be severed during surgery. This results in numbness, motor atrophy, decreased sweat production in armpit and arm.
- The medial pectoral nerve innervates pectoralis minor and the lateral portion of the pectoralis major muscles. Preservation of this nerve is particularly important to prevent atrophy of the pectoral muscles if submuscular implant reconstruction is planned.
- The thoracodorsal nerve is identifiable medial to the thoracodorsal vein. Injury may result in a weakening of the latissimus.
- The long thoracic nerve of Bell is located more medially in the axilla. It runs just beneath the fascia of the serratus anterior, medial to the thoracodorsal complex. Injury to this nerve will result in weakness in the serratus anterior muscle and cause winging of the scapula.
Pink Ribbon Program©
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
|
Information and pictures from National Cancer Institute unless otherwise specified |