Stomach / Gastric Cancer
Your Body is Your Temple
Research, Resources & Education
Table of Contents
Stomach cancer is a complex and serious disease that arises from the growth of malignant cells inside the stomach lining. These abnormal cells are able to grow and divide uncontrollably, in turn outcompeting healthy cells and eventually leading to the formation of tumors.
Information and pictures from National Cancer Institute unless otherwise specified
Stomach Anatomy & Gastric Cancer
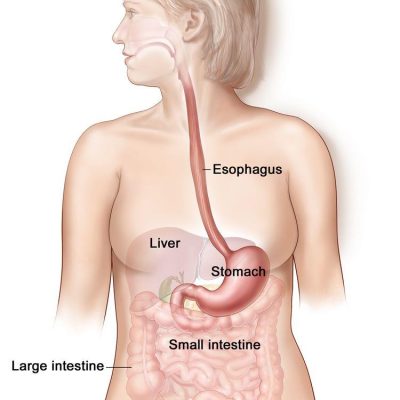
- The stomach is a J-shaped organ in the upper abdomen.
- It is part of the digestive system, which processes nutrients (vitamins, minerals, carbohydrates, fats, proteins, and water) in foods that are eaten and helps pass waste material out of the body.
- Food moves from the throat to the stomach through a hollow, muscular tube called the esophagus.
- After leaving the stomach, partly-digested food passes into the small intestine and then into the large intestine.
After gastric cancer has been diagnosed, tests are done to find out if cancer cells have spread within the stomach or to other parts of the body.
- Cancer may spread from where it began to other parts of the body.
- The following stages are used for gastric cancer:
- Stage 0 (Carcinoma in Situ)
- Stage I
- Stage II
- Stage III
- Stage IV
- Gastric cancer can recur (come back) after it has been treated.
Stomach / Gastric Cancer Videos
YouTube Videos that help explain Stomach / Gastric Cancer.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Stomach Cancer
Treatments
Also see Treatments
Surgery is a common treatment of all stages of gastric cancer. The following types of surgery may be used:
- Subtotal gastrectomy: Removal of the part of the stomach that contains cancer, nearby lymph nodes, and parts of other tissues and organs near the tumor.
- The spleen may be removed.
- The spleen is an organ that makes lymphocytes, stores red blood cells and lymphocytes, filters the blood, and destroys old blood cells.
- The spleen is on the left side of the abdomen near the stomach.
- The spleen may be removed.
- Total gastrectomy: Removal of the entire stomach, nearby lymph nodes, and parts of the esophagus, small intestine, and other tissues near the tumor.
- The spleen may be removed.
- The esophagus is connected to the small intestine so the patient can continue to eat and swallow.
If the tumor is blocking the stomach but the cancer cannot be completely removed by standard surgery, the following procedures may be used:
- Endoluminal stent placement: A procedure to insert a stent (a thin, expandable tube) in order to keep a passage (such as arteries or the esophagus) open.
- For tumors blocking the passage into or out of the stomach, surgery may be done to place a stent from the esophagus to the stomach or from the stomach to the small intestine to allow the patient to eat normally.
- Endoluminal laser therapy: A procedure in which an endoscope (a thin, lighted tube) with a laser attached is inserted into the body.
- A laser is an intense beam of light that can be used as a knife.
- Gastrojejunostomy: Surgery to remove the part of the stomach with cancer that is blocking the opening into the small intestine.
- The stomach is connected to the jejunum (a part of the small intestine) to allow food and medicine to pass from the stomach into the small intestine.
Endoscopic mucosal resection is a procedure that uses an endoscope to remove early-stage cancer and precancerous growths from the lining of the digestive tract without surgery.
- An endoscope is a thin, tube-like instrument with a light and a lens for viewing.
- It may also include tools to remove growths from the lining of the digestive tract.
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing.
- When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). (See Chemotherapy for more information)
- A type of regional chemotherapy being studied to treat gastric cancer is intraperitoneal (IP) chemotherapy.
- In IP chemotherapy, the anticancer drugs are carried directly into the peritoneal cavity (the space that contains the abdominal organs) through a thin tube.
- Hyperthermic intraperitoneal chemotherapy (HIPEC) is a treatment used during surgery that is being studied for gastric cancer.
- After the surgeon has removed as much tumor tissue as possible, warmed chemotherapy is sent directly into the peritoneal cavity.
Chemoradiation therapy combines chemotherapy and radiation therapy to increase the effects of both.
- Chemoradiation given after surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
- Chemoradiation given before surgery, to shrink the tumor (neoadjuvant therapy), is being studied.
Radiation therapy
Targeted therapy
Immunotherapy
Treatment by Stages
Also see Treatments
Treatment of stage I gastric cancer may include the following:
- Surgery (total or subtotal gastrectomy).
- Endoscopic mucosal resection for certain patients with stage IA gastric cancer.
- Surgery (total or subtotal gastrectomy) followed by chemoradiation therapy.
- Surgery and chemotherapy.
- A clinical trial of chemoradiation therapy given before surgery.
Treatment of stage II gastric cancer and stage III gastric cancer may include the following:
- Surgery (total or subtotal gastrectomy).
- Surgery and chemotherapy.
- Surgery (total or subtotal gastrectomy) followed by chemoradiation therapy or chemotherapy.
- A clinical trial of chemoradiation therapy given before surgery.
- A clinical trial of chemotherapy given before surgery.
Treatment of stage IV gastric cancer, gastric cancer that cannot be removed by surgery, or recurrent gastric cancer may include the following:
- Chemotherapy as palliative therapy to relieve symptoms and improve the quality of life.
- Targeted therapy with a monoclonal antibody with or without chemotherapy.
- Immunotherapy with pembrolizumab.
- Endoluminal laser therapy or endoluminal stent placement to relieve a blockage in the stomach, or gastrojejunostomy to bypass the blockage.
- Radiation therapy as palliative therapy to stop bleeding, relieve pain, or shrink a tumor that is blocking the stomach.
- Surgery as palliative therapy to stop bleeding or shrink a tumor that is blocking the stomach.
- Clinical trials of combinations of immunotherapy and chemotherapy.
- A clinical trial of targeted therapy with regorafenib and nivolumab.
- A clinical trial of surgery and hyperthermic intraperitoneal chemotherapy (HIPEC).
Post Gastrectomy / Side Effects
Information from Web MD – What is a Gastrectomy?
Your hospital stay will depend on the type of gastrectomy performed.
- For the first few days, you won’t be able to eat any food.
- Then you’ll be on a clear liquid diet.
- This gives your digestive tract a chance to heal.
- Instead, you’ll be fed through an IV in your vein or a catheter (tube) that goes into your belly.
- After about a week, you should be ready to start a light diet again.
- Because your stomach is smaller now, be prepared to make some changes to how you eat:
- Small meals throughout the day. Six small meals will be easier for you to digest than three large ones.
- Drink and eat at different times. Have fluids 1 hour before or after meals instead of during them.
- Watch your fiber intake. High-fiber foods like beans, lentils, and whole grains can fill you up too fast. Add them back slowly.
- Go easy on dairy. After this surgery, many people can’t digest lactose, the sugar in milk. If you’re one of them, you’ll have gas, bloating, and diarrhea after you have dairy foods.
- Take a supplement. Some nutrients like iron, calcium, and vitamins B12 and D are harder for your body to absorb from food after a gastrectomy. Your doctor may do blood tests to check these levels. If they’re low, you may need to start taking a supplement.
Dumping Syndrome. You could get what’s called dumping syndrome.
- When your small intestine has to digest a large amount of food at once, you may throw up or have nausea, cramps, or diarrhea.
- Many people notice these symptoms within an hour of eating.
- If you feel sick a few hours later, your blood sugar may be rising and falling too fast.
- It’s common to sweat, have a fast heart rate, or feel tired or confused.
- Changing what you eat can help you manage these symptoms.
- Remember, too, to be patient. After your gastrectomy, it may take 3 to 6 months to adjust. (Web MD – What is a gastrectomy?)
Risk Factors
- Having any of the following medical conditions:
- Helicobacter pylori (H. pylori) infection of the stomach.
- Chronic gastritis (inflammation of the stomach).
- Pernicious anemia.
- Intestinal metaplasia (a condition in which the normal stomach lining is replaced with the cells that line the intestines).
- Gastric polyps.
- Epstein-Barr virus infection.
- Familial syndromes (including familial adenomatous polyposis).
- Eating a diet high in salted, smoked foods and low in fruits and vegetables.
- Eating foods that have not been prepared or stored properly.
- Being older or male.
- Smoking cigarettes.
- Having a mother, father, sister, or brother who has had stomach cancer.
Recovery after Surgery
Information from CETI
Please follow MD/surgeon protocol, as every situation is unique.
Partial Gastrectomy
Hospital Stay
Full Recovery
Restrictions
Exercise
Total Gastrectomy
Hospital Stay
Full Recovery
Restrictions
Exercise
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
|
Information and pictures from National Cancer Institute unless otherwise specified |