Thyroid Cancer
Your Body is Your Temple
Research, Resources & Education
Table of Contents
Thyroid cancer is a serious illness that affects the thyroid gland - an essential organ that regulates many important bodily functions. This disease is caused by the formation of malignant (cancerous) cells within the thyroid gland, resulting in the growth of tumors and the potential spread of cancerous cells throughout the body. Signs and symptoms of thyroid cancer may include changes in the size or shape of the thyroid gland, difficulty swallowing, hoarseness or other changes in voice quality, and swollen lymph nodes in the neck.
|
Information and pictures from National Cancer Institute unless otherwise specified |
Thyroid Anatomy and Hormones
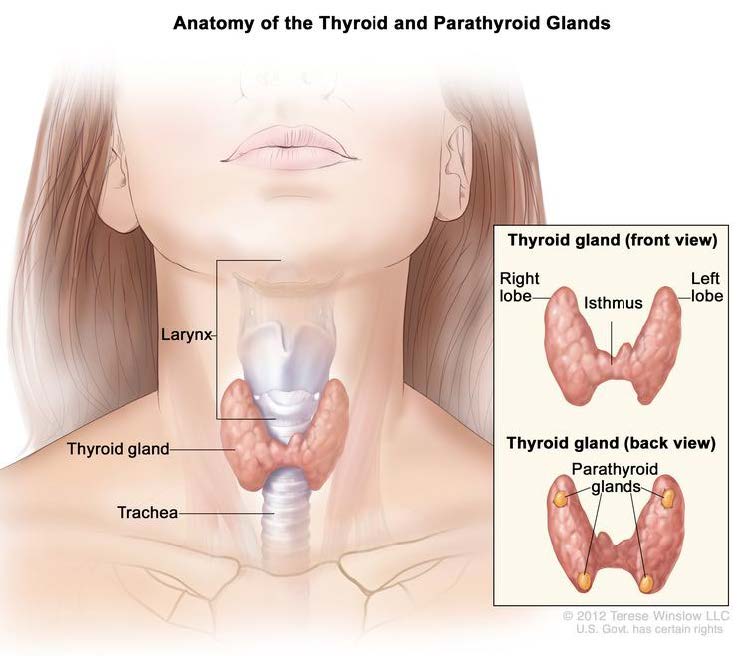
The thyroid is a gland at the base of the throat near the trachea (windpipe).
- It is shaped like a butterfly, with a right lobe and a left lobe.
- The isthmus, a thin piece of tissue, connects the two lobes.
- A healthy thyroid is a little larger than a quarter.
- It usually cannot be felt through the skin.
- The thyroid uses iodine, a mineral found in some foods and in iodized salt, to help make several hormones.
- The parathyroid glands are four pea-sized organs found in the neck near the thyroid.
- The thyroid and parathyroid glands make hormones.
Thyroid hormones do the following:
- Control heart rate, body temperature, and how quickly food is changed into energy (metabolism).
- Control the amount of calcium in the blood.
Thyroid Cancer Videos
YouTube Videos that help explain Thyroid Cancer.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Thyroid Cancer
Types of Thyroid Cancer and Stages
- The most common type of thyroid cancer.
- Well-differentiated tumors (papillary thyroid cancer and follicular thyroid cancer) can be treated and can usually be cured.
Well-differentiated tumors (papillary thyroid cancer and follicular thyroid cancer) can be treated and can usually be cured.
Cancer that develops in C cells of the thyroid.
- The C cells make a hormone (calcitonin) that helps maintain a healthy level of calcium in the blood.
- Medullary thyroid cancer is a neuroendocrine tumor that forms from cells that release hormones into the blood in response to a signal from the nervous system.
- Neuroendocrine tumors may make higher-than-normal amounts of hormones, which can cause many different symptoms.
- These tumors may be benign (not cancer) or malignant (cancer).
- Poorly differentiated and undifferentiated tumors (anaplastic thyroid cancer) are less common.
- These tumors grow and spread quickly and have a poorer chance of recovery.
- Patients with anaplastic thyroid cancer should have molecular testing for a mutation in the BRAF gene.
- Papillary and follicular thyroid cancer are sometimes called differentiated thyroid cancer.
- Medullary and anaplastic thyroid cancer are sometimes called poorly differentiated or undifferentiated thyroid cancer.
Stages are used to describe thyroid cancer based on the type of thyroid cancer and the age of the patient:
- Papillary and follicular thyroid cancer in patients younger than 55 years
- Papillary and follicular thyroid cancer in patients 55 years and older
- Anaplastic thyroid cancer in patients of all ages
- Medullary thyroid cancer in patients of all ages
- Thyroid cancer can recur (come back) after it has been treated.
Treatments
Also see Treatments
Surgery is the most common treatment for thyroid cancer. One of the following procedures may be used:
- Lobectomy: Removal of the lobe in which thyroid cancer is found.
- Lymph nodes near the cancer may also be removed and checked under a microscope for signs of cancer.
- Near-total thyroidectomy: Removal of all but a very small part of the thyroid.
- Lymph nodes near the cancer may also be removed and checked under a microscope for signs of cancer.
- Total thyroidectomy: Removal of the whole thyroid.
- Lymph nodes near the cancer may also be removed and checked under a microscope for signs of cancer.
- Tracheostomy: Surgery to create an opening (stoma) into the windpipe to help you breathe.
- The opening itself may also be called a tracheostomy.
Radiation therapy may be given after surgery to kill any thyroid cancer cells that were not removed.
Follicular and papillary thyroid cancers are sometimes treated with radioactive iodine (RAI) therapy.
- RAI is taken by mouth and collects in any remaining thyroid tissue, including thyroid cancer cells that have spread to other places in the body.
- Since only thyroid tissue takes up iodine, the RAI destroys thyroid tissue and thyroid cancer cells without harming other tissue.
- Before a full treatment dose of RAI is given, a small test-dose is given to see if the tumor takes up the iodine.
In the treatment of thyroid cancer, drugs may be given to prevent the body from making thyroid- stimulating hormone (TSH), a hormone that can increase the chance that thyroid cancer will grow or recur.
- Also, because thyroid cancer treatment kills thyroid cells, the thyroid is not able to make enough thyroid hormone.
- Patients are given thyroid hormone replacement pills.
Targeted therapy
Chemotherapy
Watchful waiting
Possible Side Effects
Tracheostomy Side Effect Information from John Hopkins Medicine – Tracheostomy
SURGERY
- Total Thyroidectomy:
- Pain and aches in neck and shoulders
- Will need to be on replacement medication
- Hoarseness
- Sore throat
- Difficulty swallowing
- Transient (temporary) hypoparathyroidism can happen after thyroid surgery. Hypoparathyroidism is when you have too little parathyroid hormone, which can lead to low calcium levels.
- Tracheostomy:
- Bleeding
- Air trapped around the lungs (pneumothorax)
- Air trapped in the deeper layers of the chest(pneumomediastinum)
- Air trapped underneath the skin around the tracheostomy (subcutaneous emphysema)
- Damage to the swallowing tube (esophagus)
- Injury to the nerve that moves the vocal cords (recurrent laryngeal nerve)
- Tracheostomy tube can be blocked by blood clots, mucus or pressure of the airway walls. Blockages can be prevented by suctioning, humidifying the air, and selecting the appropriate tracheostomy tube. (John Hopkins – Complications and Risks of Tracheostomy)
Radioactive Iodine Treatment
- Dry eyes
- Dry mouth
- Salivary gland swelling or pain
- Neck swelling and pain
Radiation to the neck
- Dry, sore mouth and throat
- Hoarseness
- Difficulty swallowing
- Fatigue
Risk Factors
- Being between 25 and 65 years old.
- Being female.
- Being exposed to radiation to the head and neck as an infant or child or being exposed to radioactive fallout. The cancer may occur as soon as 5 years after exposure.
- Having a history of goiter (enlarged thyroid).
- Having a family history of thyroid disease or thyroid cancer.
- Having certain genetic conditions such as familial medullary thyroid cancer (FMTC), multiple endocrine neoplasia type 2A syndrome (MEN2A), or multiple endocrine neoplasia type 2B syndrome (MEN2B).
- Being Asian.
Recovery after Surgery
Information from CETI
Please follow MD/surgeon protocol, as every situation is unique.
Thyroidectomy - Total
Hospital Stay
Full Recovery
Restrictions
No lifting over 10 lbs for 2 or more weeks.
Exercise
Tracheostomy
Hospital Stay
Full Recovery
Restrictions
No lifting over 5 lbs. for at least weeks.
Exercise
Recommendations
- Start exercises or stretches after clearance from MD.
- You may have some minor muscle spasms in the upper back and neck.
- It will be important for you to keep these muscles relaxed, and to maintain normal posture as much as possible to reduce these spasms.
- Your voice may sound different for a few days to weeks after the surgery.
- Some patients are hoarse and some have “voice fatigue,” meaning their voice is “tired” at the end of the day.
- There are a small percentage of patients that will need special voice therapy if your voice does not return in 6-8 weeks.
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
|
Information and pictures from National Cancer Institute unless otherwise specified |