Central Nervous System / Brain Cancer
Your Body is Your Temple
Research, Resources & Education
Table of Contents
Adult central nervous system tumor is a complex condition that poses a significant threat to an individual's neurological health, affecting the proper functioning of the brain and spinal cord - the two primary components of the central nervous system (CNS). The disease is caused by the formation of abnormal cells in these regions that disrupt the normal flow of electrical impulses through the body, leading to various symptoms that can substantially impact an individual's quality of life. These abnormal cells can grow and divide rapidly, forming mass or lumps that can expand and press on vital brain structures, causing severe damage or impairment.
Information and pictures from National Cancer Institute unless otherwise specified
Brain & Spinal Cord Description
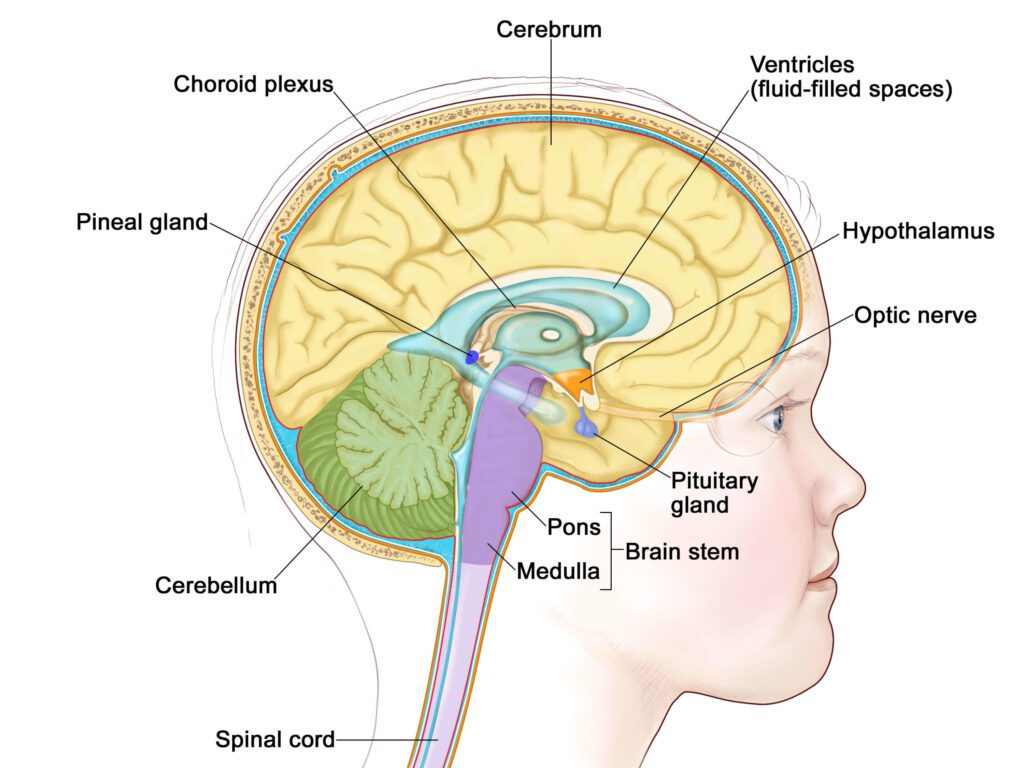
The brain controls many important body functions. The brain has three major parts:
- The cerebrum is the largest part of the brain. It is at the top of the head. The cerebrum controls thinking, learning, problem solving, emotions, speech, reading, writing, and voluntary movement.
- The cerebellum is in the lower back of the brain (near the middle of the back of the head). It controls movement, balance, and posture.
- The brain stem connects the brain to the spinal cord. It is in the lowest part of the brain (just above the back of the neck). The brain stem controls breathing, heart rate, and the nerves and muscles used to see, hear, walk, talk, and eat.
The spinal cord connects the brain to nerves in most parts of the body.
- The spinal cord is a column of nerve tissue that runs from the brain stem down the center of the back.
- It is covered by three thin layers of tissue called membranes. These membranes are surrounded by the vertebrae (back bones).
- Spinal cord nerves carry messages between the brain and the rest of the body, such as a message from the brain to cause muscles to move or a message from the skin to the brain to feel touch.
Brain Tumor Videos
YouTube Videos that help explain types of Brain Cancer.
Disclaimer:
This is for research only and Lost Temple Fitness & Cancer does not endorse any video presented on this website.
It is advised that you ALWAYS CHECK WITH YOUR PHYSICIAN for a proper diagnosis and treatment plan.
Brain Cancer / Tumors
0:16
Benign or Malignant
Benign
Malignant
Benign & Malignant Tumors
Metastatic Brain Tumors
A tumor that starts in another part of the body and spreads to the brain is called a metastatic brain tumor (or brain metastases). Metastatic brain tumors are more common than primary brain tumors.
Tumors that start in the brain are called primary brain tumors. Primary brain tumors may spread to other parts of the brain or to the spine. They rarely spread to other parts of the body.
Up to half of metastatic brain tumors are from lung cancer. Other types of cancer that commonly spread to the brain include:
- Melanoma.
- Breast cancer.
- Colon cancer.
- Kidney cancer.
- Nasopharyngeal cancer.
- Cancer of unknown primary site.
Cancer may spread to the leptomeninges (the two innermost membranes covering the brain and spinal cord). This is called leptomeningeal carcinomatosis. The most common cancers that spread to the leptomeninges include:
- Breast cancer.
- Lung cancer.
- Leukemia.
- Lymphoma.
There are different types of brain and spinal cord tumors.
- Brain and spinal cord tumors are named based on the type of cell they formed in and where the tumor first formed in the CNS.
- The grade of a tumor may be used to tell the difference between slow-growing and fast-growing types of the tumor.
- The World Health Organization (WHO) tumor grades are based on how abnormal the cancer cells look under a microscope and how quickly the tumor is likely to grow and spread.
WHO Tumor Grading System
Grade I
Grade II
Grade III
Grade IV
Treatments for Brain/CNS Cancer
Also see Treatments
Surgery may be used to diagnose and treat adult brain and spinal cord tumors.
- Removing tumor tissue helps decrease pressure of the tumor on nearby parts of the brain.
- After the doctor removes all the cancer that can be seen at the time of the surgery, some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left.
- Treatment given after the surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
- To treat brain tumors, a wafer that dissolves may be used to deliver a chemotherapy drug directly to the brain tumor site after the tumor has been removed by surgery.
- The way the chemotherapy is given depends on the type and grade of tumor and where it is in the brain.
Other types of targeted therapies are being studied for adult brain tumors, including tyrosine kinase inhibitors and new VEGF inhibitors.
- A type of high-energy, external radiation therapy that uses streams of protons (tiny particles with a positive charge) to kill tumor cells.
- This type of treatment can lower the amount of radiation damage to healthy tissue near a tumor.
- It is used to treat cancers of the head, neck, and spine and organs such as the brain, eye, lung, and prostate.
- Proton beam radiation is different from x-ray radiation.
Immunotherapy is being studied for the treatment of some types of brain tumors. Treatments may include the following:
- Dendritic cell vaccine therapy.
- Gene therapy.
- Active surveillance
- Radiation therapy
- Supportive care is given to lessen the problems caused by the disease or its treatment
Type & Treatment of Primary Adult Brain Tumors
Also see Treatments
An astrocytic tumor begins in star-shaped brain cells called astrocytes, which help keep nerve cells healthy. An astrocyte is a type of glial cell. Glial cells sometimes form tumors called gliomas.
A tumor located in the part of the brain that connects to the spinal cord (the brain stem).
- It may grow rapidly or slowly, depending on the grade of the tumor.
- It is often a high-grade tumor, which spreads widely through the brain stem.
- Brain stem gliomas are rare in adults.
Treatment of brain stem gliomas may include the following:
- Radiation therapy.
A pineal astrocytic tumor forms in tissue around the pineal gland and may be any grade.
- The pineal gland is a tiny organ in the brain that makes melatonin, a hormone that helps control the sleeping and waking cycle
Treatment of pineal astrocytic tumors may include the following:
- Surgery
- Radiation therapy.
- For high-grade tumors, chemotherapy may also be given.
A pilocytic astrocytoma grows slowly in the brain or spinal cord. It may be in the form of a cyst and rarely spreads into nearby tissues.
Treatment of pilocytic astrocytomas may include the following:
- Surgery to remove the tumor.
- Radiation therapy may also be given if tumor remains after surgery.
A diffuse astrocytoma grows slowly, but often spreads into nearby tissues.
- The tumor cells look something like normal cells.
- It is also called a low-grade diffuse astrocytoma.
Treatment of diffuse astrocytomas may include the following:
- Surgery with or without radiation therapy.
- Surgery followed by radiation therapy and chemotherapy.
An anaplastic astrocytoma grows quickly and spreads into nearby tissues.
- The tumor cells look different from normal cells.
- An anaplastic astrocytoma is also called a malignant astrocytoma or high-grade astrocytoma.
Treatment of anaplastic astrocytomas may include the following:
- Surgery and radiation therapy.
- Chemotherapy may also be given.
- Surgery and chemotherapy.
- A clinical trial of chemotherapy placed into the brain during surgery.
- A clinical trial of a new treatment added to standard treatment.
A glioblastoma grows and spreads very quickly. The tumor cells look very different from normal cells.
- A fast-growing type of central nervous system tumor that forms from glial (supportive) tissue of the brain and spinal cord and has cells that look very different from normal cells.
- Glioblastoma usually occurs in adults and affects the brain more often than the spinal cord.
- Also called GBM, glioblastoma multiforme, and grade IV astrocytoma.
Treatment of glioblastomas may include the following:
- Surgery followed by radiation therapy and chemotherapy given at the same time, followed by chemotherapy alone.
- Surgery followed by radiation therapy.
- Chemotherapy placed into the brain during surgery.
- Radiation therapy and chemotherapy given at the same time.
- A clinical trial of a new treatment added to standard treatment.
An oligodendroglial tumor begins in brain cells called oligodendrocytes, which help keep nerve cells healthy. An oligodendrocyte is a type of glial cell. Oligodendrocytes sometimes form tumors called oligodendrogliomas. Grades of oligodendroglial tumors include the following: • Oligodendroglioma (grade II): An oligodendroglioma grows slowly, but often spreads into nearby tissues. The tumor cells look something like normal cells. • Anaplastic oligodendroglioma (grade III): An anaplastic oligodendroglioma grows quickly and spreads into nearby tissues. The tumor cells look different from normal cells.
Treatment of oligodendrogliomas may include the following:
- Surgery with or without radiation therapy.
- Chemotherapy may be given after radiation therapy.
Treatment of anaplastic (a term used to describe cancer cells that divide rapidly and have little or no resemblance to normal cells) oligodendroglioma may include the following:
- Surgery followed by radiation therapy with or without chemotherapy.
- A clinical trial of a new treatment added to standard treatment.
A mixed glioma is a brain tumor that has two types of tumor cells in it — oligodendrocytes and astrocytes.
- This type of mixed tumor is called an oligoastrocytoma.
Treatment of mixed gliomas may include the following:
- Surgery and radiation therapy.
- Sometimes chemotherapy is also given.
Oligoastrocytoma (grade II): An oligoastrocytoma is a slow-growing tumor.
- The tumor cells look something like normal cells. .
Anaplastic oligoastrocytoma (grade III): An anaplastic oligoastrocytoma grows quickly and spreads into nearby tissues.
- The tumor cells look different from normal cells.
- This type of tumor has a worse prognosis than oligoastrocytoma (grade II).
An ependymal tumor usually begins in cells that line the fluid-filled spaces in the brain and around the spinal cord.
- An ependymal tumor may also be called an ependymoma.
Ependymoma (grade I or II): A grade I or II ependymoma grows slowly and has cells that look something like normal cells.
- There are two types of grade I ependymoma — myxopapillary ependymoma and subependymoma.
- A grade II ependymoma grows in a ventricle (fluid-filled space in the brain) and its connecting paths or in the spinal cord.
Treatment of grade I and grade II ependymomas may include the following:
- Surgery to remove the tumor.
- Radiation therapy may also be given if tumor remains after surgery.
Anaplastic ependymoma (grade III): An anaplastic ependymoma grows quickly and spreads into nearby tissues.
- The tumor cells look different from normal cells.
- This type of tumor usually has a worse prognosis than a grade I or II ependymoma.
Treatment of grade III anaplastic ependymoma may include the following:
- Surgery and radiation therapy.
- A fast-growing type of cancer that forms in the cerebellum (the lower, back part of the brain).
- Medulloblastomas tend to spread through the cerebrospinal fluid to the spinal cord or to other parts of the brain. They may also spread to other parts of the body, but this is rare.
- Medulloblastomas are most common in children and young adults.
- They are a type of central nervous system embryonal tumor.
- Surgery and radiation therapy to the brain and spine.
- A clinical trial of chemotherapy added to surgery and radiation therapy to the brain and spine
A pineal parenchymal tumor forms in parenchymal cells or pineocytes, which are the cells that make up most of the pineal gland.
- These tumors are different from pineal astrocytic tumors.
Grades of pineal parenchymal tumors include the following:
- Pineocytoma (grade II): A pineocytoma is a slow-growing pineal tumor.
- Pineoblastoma (grade IV): A pineoblastoma is a rare tumor that is very likely to spread.
- For pineocytomas, surgery and radiation therapy.
- For pineoblastomas, surgery, radiation therapy, and chemotherapy.
A meningeal tumor, also called a meningioma, forms in the meninges (thin layers of tissue that cover the brain and spinal cord).
- It can form from different types of brain or spinal cord cells.
- Meningiomas are most common in adults.
Types of meningeal tumors include the following:
- Meningioma (grade I): A grade I meningioma is the most common type of meningeal tumor.
- A grade I meningioma is a slow-growing tumor.
- It forms most often in the dura mater.
- A grade I meningioma may be completely removed by surgery.
- Meningioma (grade II and III): This is a rare meningeal tumor.
- It grows quickly and is likely to spread within the brain and spinal cord.
- The prognosis is worse than a grade I meningioma because the tumor usually cannot be completely removed by surgery.
- A Hemangiopericytoma is not a meningeal tumor but is treated like a grade II or III meningioma.
- A hemangiopericytoma usually forms in the dura mater.
- The prognosis is worse than a grade I meningioma because the tumor usually cannot be completely removed by surgery.
Treatment of grade I meningiomas may include the following:
- Active for tumors with no signs or symptoms.
- Surgery to remove the tumor.
- Radiation therapy may also be given if tumor remains after surgery.
- Stereotactic radiosurgery for tumors smaller than 3 centimeters.
- Radiation therapy for tumors that cannot be removed by surgery.
Treatment of grade II and III meningiomas and hemangiopericytomas may include the following:
- Surgery and radiation therapy.
A germ cell tumor forms in germ cells, which are the cells that develop into sperm in men or ova (eggs) in women.
- There are different types of germ cell tumors. These include germinomas, teratomas, embryonal yolk sac carcinomas, and choriocarcinomas.
- Germ cell tumors can be either benign or malignant.
- There is no standard treatment for germ cell tumors (germinoma, embryonal carcinoma, choriocarcinoma, and teratoma).
- Treatment depends on what the tumor cells look like under a microscope, the tumor markers, where the tumor is in the brain, and whether it can be removed by surgery.
A craniopharyngioma is a rare tumor that usually forms in the center of the brain just above the pituitary gland (a pea-sized organ at the bottom of the brain that controls other glands).
- Craniopharyngiomas can form from different types of brain or spinal cord cells.
- Craniopharyngiomas are slow-growing and do not spread to other parts of the brain or to other parts of the body.
- However, they may grow and press on nearby parts of the brain, including the pituitary gland, hypothalamus, optic chiasm, optic nerves, and fluid-filled spaces in the brain. This may cause problems with growth, vision, and making certain hormones.
- Craniopharyngiomas usually occur in children and young adults.
Treatment of craniopharyngiomas may include the following:
- Surgery to completely remove the tumor.
- Surgery to remove as much of the tumor as possible, followed by radiation therapy.
Treatment of spinal cord tumors may include the following:
- Surgery to remove the tumor.
- Radiation therapy.
- A clinical trial of a new treatment.
There is no standard treatment for recurrent central nervous system (CNS) tumors.
- Treatment depends on the patient’s condition, the expected side effects of the treatment, where the tumor is in the CNS, and whether the tumor can be removed by surgery.
Treatment may include the following:
- Chemotherapy placed into the brain during surgery.
- Chemotherapy with drugs not used to treat the original tumor.
- Targeted therapy for recurrent glioblastoma.
- Radiation therapy.
- Surgery to remove the tumor.
- A clinical trial of a new treatment.
Treatment of one to four tumors that have spread to the brain from another part of the body may include the following:
- Radiation therapy to the whole brain with or without surgery.
- Radiation therapy to the whole brain with or without stereotactic radiosurgery.
- Stereotactic radiosurgery.
- Chemotherapy, if the primary tumor is one that responds to anticancer drugs. It may be combined with radiation therapy.
Treatment of tumors that have spread to the leptomeninges may include the following:
- Chemotherapy (systemic and/or intrathecal).
- Radiation therapy may also be given.
- Supportive care.
Risk Factors, Side Effects and Late Side Effects
Risk Factors
- Being exposed to vinyl chloride may increase the risk of glioma.
- Infection with the Epstein-Barr virus, having AIDS (acquired immunodeficiency syndrome), or receiving an organ transplant may increase the risk of primary CNS lymphoma.
- Having certain genetic syndromes may increase the risk brain tumors:
- Neurofibromatosis type 1 (NF1) or 2 (NF2).
- Von Hippel-Lindau disease.
- Tuberous sclerosis.
- Li-Fraumeni syndrome.
- Turcot syndrome type 1 or 2.
- Nevoid basal cell carcinoma syndrome.
Side Effects
- Weakness.
- Dizzy spells.
- Poor balance or lack of coordination.
- Personality or behavior changes.
- Confusion.
- Problems with your speech.
Other Side Effects
- Infections
- Bleeding
- Seizures
- Stoke
- Headaches
- Neck Stiffness
- Brain Swelling
- Coma
- Brain Damage
- Damage to healthy tissues
Recovery After Surgery
Information from CETI
Please follow MD/surgeon protocol, as every situation is unique.
Hospital Stay
Full Recovery
Restrictions
Exercise
Balance - Exercise Precautions
Medical Clearance
Start Slow
Stability
Solid Surface
No Quick Movements
Safety First
Disclaimer: The information in this book/website is for educational purposes only and has been obtained through research, publications and personal experience, and shall not be liable for incorrect information. Any mentioned publications or websites does not imply endorsement. As this industry is ever changing, I urge readers to confirm the information contained in this book/website. The author will not be liable for any injuries sustained from practicing techniques taught or for any typographical errors or omissions.
It is advised that you always check with your medical doctor or physical therapist before starting an exercise program or change in diet.
|
Information and pictures from National Cancer Institute unless otherwise specified |